Article
Researchers Scrutinize High Discontinuation Rates of Statins
Author(s):
Though many patients indicate side effects as the reason they stop taking their prescribed statins, clinical trials have not documented high discontinuation rates due to adverse drug reactions.
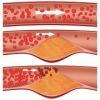
It seems as though everyone has hypercholesterolemia. In fact, it’s the most common chronic condition in the United States. It’s also highly responsive to drug intervention, the most common of which is a prescription for a 3-Hydroxy-3-methylglutaryl coenzyme A reductase inhibitor, or statin.
Statins improve patients’ cholesterol panels remarkably, and they have been proven to decrease mortality in patients who have high cholesterol. Regardless, many patients stop taking their prescribed statins, often indicating that they cannot tolerate the side effects. Since clinical trials have not documented high discontinuation rates due to adverse drug reactions (ADRs), that raises several questions: Do patients experience more ADRs to statins in real-world settings than in clinical trials? Are the events those patients experience actually associated with the statin, or something else? Would switching to a different statin be associated with fewer ADRs?
A new study published in the Annals of Internal Medicine has uncovered the factors that lead to statin discontinuation. Using structured electronic medical record entries and analyses of electronic provider notes, the researchers, who were associated with Brigham and Women’s Hospital and Massachusetts General Hospital, amassed records for adult patients who had at least one statin prescription between January 2000 and December 2008 (n=107,835).
Of the 57,292 patients whose statin therapy was discontinued at least once, 69.1 percent had electronic chart entries that explained the reason. Clinicians most often indicated that the statin was “no longer necessary,” which was also the default explanation in the software and a reason that clinicians often cite regardless of the real motive. Additionally, 3.8 percent of the patients who discontinued statin therapy cited an adverse reaction as the reason. Among all 107,835 patients, nearly 18 percent reported statin-related events — which was significantly higher than the rates reported in clinical trials — and about 40 percent of those side effects were described as musculoskeletal symptoms. Mild creatine kinase (CK) elevations were not associated with difficulty tolerating the drug, and rhabdomyolysis and memory loss were only rarely reported.
After they were re-challenged with a different statin, most patients were able to tolerate the new drug. However, the study authors reminded prescribers to take a conservative approach and advise patients who experience tolerable myalgia with a less than 10-fold CK elevation to remain on statin therapy. They also suggested re-challenging patients with the same statin after a break from treatment or a different statin in the patients have ADRs.
Regardless of the selected approach, the authors said permanent discontinuation of statins is unwise, especially in patients who have risk factors for cardiac disease.




