Publication
Article
Cardiology Review® Online
Use of Secondary Prevention Drugs for Cardiovascular Disease in the Community
Author(s):

Karla K. Quevedo, MD
REVIEW
Yusuf S, Islam S, Chow CK, et al. Use of secondary prevention drugs for cardiovascular dis- ease in the community in high-income, middle-income, and low-income countries (the PURE Study): a prospective epidemiological survey [published online ahead of print August 28, 2011]. Lancet. doi:10.1016/S0140-6736(11)61215-4.
Cardiovascular disease (CVD) remains the leading cause of death in the world, and approximately 80% of all cardiovascular deaths occur in low- and middle-income countries and in younger patients in compari- son with patients’ ages in high-income countries.1 Many studies have shown that the regular use of β-blockers, an- giotensin-converting-enzyme (ACE) inhibitors, and antiplatelet drugs reduce death, reinfarction, or stroke in patients with coronary heart disease.2 Treatment rates for individuals with prevalent coronary heart disease or stroke in the community are unknown because many people cannot afford medical care long- term after the acute event. Most currently available data on treatment rates are from high-income countries.
The Prospective Urban Rural Epide- miological (PURE) study was designed to assess rates of use of medications proved effective for secondary prevention in populations with prevalent CVD from urban and rural communities in high-, middle-, and low-income countries.
Study Details
The PURE study was based on a prospec- tive epidemiological survey. Using World Bank classifications in place at the time the PURE study was started, the authors included 4 low-income countries (Bangla- desh, India, Pakistan, and Zimbabwe), 7 upper-middle-income countries (Argentina, Brazil, Chile, Malaysia, Poland, South Africa, and Turkey), 3 lower-middle-income countries (China, Colombia, and Iran), and 3 high-income countries (Canada, Sweden, and United Arab Emirates). Within every country, an urban and rural community was selected at collaborating sites on the basis of previously published studies. All data were entered in a customized database programmed with range and consistency checks and transmitted electronically to the project office at the Population Health Research Institute in Hamilton, Ontario, Canada, where further quality-control measures were implemented.
History of cardiovascular and other diseases was assessed with standardized questionnaires; 89% of the information collected during central adjudication was confirmed with medical or hospital records. The use of antiplatelet drugs, β-blockers, ACE inhibitors or angiotensin-receptor blockers (ARBs), statins, and diuretics was analyzed. The study also included β-blockers and ACE inhibitors or ARBs, diuretics, or calcium channel blockers in an analysis of blood-pressure-lowering drugs.
The study recruited 382,341 individuals from 107,599 households in 628 communities (348 urban and 280 rural) in 17 countries on 5 continents. Recruitment started in Karnataka, India, in January 2003. A total of 197,332 (52%) individuals were eligible for the main study, and 153,662 adults agreed to participate in the adult study. Complete measurements and questionnaires were provided by 151,966 of 153,662 individuals.
Characteristics of the 197,332 eligible adults and the 153,578 participants aged 35 to 70 years with complete data were similar in both groups (mean age, sex, level of education, smoking status, history of hypertension, stroke, coronary heart disease, cancer, and diabetes). A total of 5650 participants had a self-reported coronary heart disease event (median, 5.0 years previously [interquartile range (IQR), 2.0-10.0]) and 2292 had a stroke event (4.0 years previously [IQR, 2.0-8.0]).
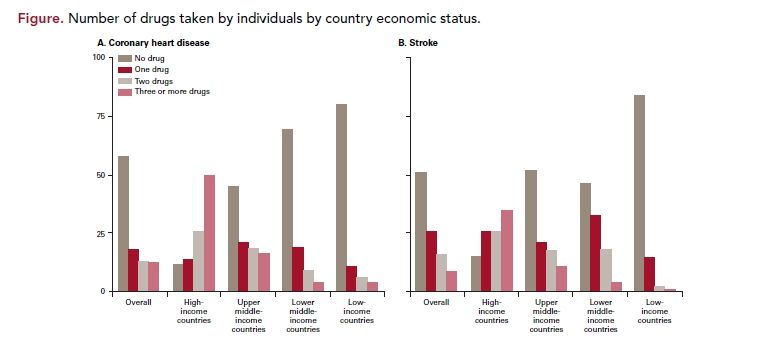
Among patients who had coronary heart disease or stroke, 58.5% were not taking any of the 4 drugs proved effective, and 3.1% were taking all 4 types of drugs. Fewest patients received none of the drugs in high-income countries (11.2%), compared with 45.1% in upper-middle-income countries, 69.3% in lower-middle-income countries, and 80.2% in low-income countries. Overall, few individuals with CVD were taking antiplatelet drugs (25.3%), β-blockers (17.4%), ACE inhibitors or ARBs (19.5%), or statins (14.6%) (Figure).
There was a strong correlation between overall rates of drug use and per-head health expenditure by country and gross domestic product. The overall rates of use of secondary prevention drugs were higher in urban areas than in rural areas. Patients younger than 60 years were less likely to take the drugs than were patients 60 years or older (31.9% of patients 60 years or older vs 26.6% of those aged 50-60 years). Women were less likely to take drugs proved effective after coronary heart dis- ease than were men. Patients who had the highest level of education were more likely to take antiplatelet drugs or statins than were those with the lowest level of education. Use of drugs proved to be effective was consistently lower in current smokers than it was in former smokers or those who never smoked. These patterns were consistent for all country economic statuses, and rates for all drug types were lowest in smokers from low- income countries. Country-level factors affected rates of drug use more than did individual-level factors.
The PURE study provided prospective data for individuals in numerous countries from urban and rural settings in high-income, middle-income, and low- income countries. The use of secondary prevention drugs for CVD was assessed in this study, demonstrating a substantial shortfall in the use of proved-effective, inexpensive medications (aspirin, β-blockers, ACE inhibitors or ARBs, diuretics, or statins) in patients with coronary heart disease or stroke in all countries studied, with the greatest shortfalls in low-income countries.
References
1. Gersh BJ, Sliwa K, Mayosi B, Yusuf S. Novel therapeutic concepts: the epidemic of cardiovascular disease in the developed world: global implications. Eur Heart J. 2010;31:642-648.
2. Weiner SD, Rabbani LE. Secondary pre- vention strategies for coronary heart disease. J Thromb Thrombolysis. 2010;29:8-24.
3. Kreatsoulas C, Anand S. The impact of so- cial determinants on cardiovascular disease. Can J Cardiol. 2010; 26 (suppl C):8C-13C.
4. O’Donnell MJ, Xavier D, Liu L, et al. Risk factors for ischemic and intracerebral hemorrhagic stroke in 22 countries (the IN- TERSTROKE study): a case-control study. Lancet. 2010;376:112-123.
5. Yusuf S, Hawken S, Ounpuu S, et al. Ef- fect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case- control study. Lancet. 2004;364:937-952.
6. Smith SC, Allen J, Blair S, et al. AHA/ ACC Guidelines for secondary prevention for patients with coronary and other ath- erosclerotic vascular disease: 2006 update endorsed by the National Heart, Lung, and Blood Institute. J Am Coll Cardiol. 2006;47:2130-2139.
7. Gupta R, Deedwania P. Interventions for cardiovascular disease prevention. Cardiol Clin. 2011;29:15-34.
8. Mendis S, Abegunde D, Yusuf S, et al. WHO study on prevention of REcurrences of myocardial infarction and strokE (WHO- PREMISE). Bull World Health Organ. 2005;83:820-829.
9. Jeemon P, Reddy KS. Social determinants of cardiovascular disease outcomes in Indi- ans. Indian J Med Res. 2010;132(5):617-622.
10. Neubeck L, Redfern J, Briffa T, Bauman A, Hare D, Freedman SB. The CHOICE (Choice of Health Options In Prevention of Cardiovas- cular Events) replication trial: study protocol. BMC Cardiovasc Disord. 2008;8:25.
11. Bailey TC, Noirot LA, Gage BF, et al. Im- proving adherence to coronary heart disease secondary prevention medication guidelines at a community hospital.
COMMENTARY
Medications and Secondary Prevention
C
ardiology CVD is the leading cause of morbidity and mor- tality among high-income countries of the industrialized world and the leading cause of noncommunicable morbidity and mortality among low- and middle-income countries, accounting for almost 25% of total deaths.3 By the year 2030, CVD is projected to be the leading cause of death worldwide.3
One of the most important achievements in cardiovas- cular research has been the identification of risk factors associated with CVD, with subsequent development of treatments to modify these risk factors. The INTERSTROKE study reported that 10 common risk factors explained more that 90% of incident hemorrhagic and thrombotic strokes.4 The INTERHEART study similarly found that more than 90% of the population-attributable risk for myocardial infarction can be explained by 9 modifiable risk factors: ratio of apolipoprotein B/apolipoprotein A, smoking, diabetes, hypertension, central obesity, psychosocial factors, fruit/vegetable consum tion, physical activity, and alcohol use.5 Recommendations to modify risk factors have been published by the American Heart Association in the Guidelines for Secondary Prevention for Patients with Coronary and Other Atherosclerotic Vascular Disease.6
There is strong evidence to support aggressive risk fac tor management to improve survival and reduce recur- rent events and the need for interventional procedures in patients with established CVD. However, despite advances in secondary prevention of CVD, there are still gross deficiencies in cardiovascular health care.
A limitation of the PURE Study is that the diagnosis of coronary heart disease and stroke were self-reported, so a proportion of patients may not have had vascular disease. Patients older than 70 years of age were excluded—an important demographic with a high incidence of CVD. Medication use was also self-reported and did use more objective methods, which may be a poor reflection of actual use.
Despite these limitations, PURE demonstrates that there is a worldwide underuse of effective drugs for secondary prevention of CVD. Could this be contributing to the global phenomenon of the epidemic of CVD? This is a critical question that needs to be considered in further research studies. Explanations for the poor medication compliance found in the study are still not clear. The fact that many of the effective drugs are currently inexpensive and that a high percentage of underuse was also found in patients with access to medical care make this issue a complicated one. In order to have a clearer explanation for the underuse of effective drugs, more prospective studies are needed, using multinational, national, and community databases and using countries at various economic stages.
Because of the increasing incidence of CVD, it is crucial that we also understand the social and economic factors affecting this disease. The social determinants of health, such as place of residence, race, ethnicity, gender, education, and socioeconomic status, need to be taken into consideration.7-9 Unfortunately, there is not 1 global solution to the problem.
While many challenges remain for primary and sec- ondary prevention, approaches include public health/ community-based strategies focused on risk factors and, alternatively, clinic-based strategies focused on targeting high-risk subgroups. Different protocols have already been studied, such as a telephone follow-up program after a vascular event (CHOICE study)10 and a technology- assisted pharmacist intervention to improve physician adherence to secondary prevention guidelines.11 All of these interventions have shown promising results, with the goal of decreasing complications of CVD. New strat- egies that have been successful need to be implemented according to the needs of the individual community, and only with this targeted strategy may we be able to im- prove population health and reduce the burden placed on health care resources related to CVD.
About the Author
Karla k. Quevedo, MD, is a third-year resident in Internal Medicine at Texas Tech University Health Science Center in El Paso, Texas. Dr. Quevedo received her MD at the Universidad San Martin de Porres in Peru in 2003. She was chief resident in internal medicine at Guillermo Almenara Hospital in Lima, Peru. Her areas of interest are general cardiology, preventive cardiology, and heart failure and biomarkers.
