Publication
Article
Family Practice Recertification
Why Does This Woman Have Punched-out Bone Lesions?
Author(s):
When a patient's presenting complaint is chest pain, consider plain radiographs directed to the area of pain and do not forget to look at the bones.
James D. Collins, MD
This 35-year-old woman had fallen while moving from her wheelchair to her bed. When she fell, she struck her head on a chair, lost her sense of direction, and injured her left hip. She then complained of rib pain that worsened with movement.
Her medical history included recurrent bacterial infections, and physical examination found kyphosis of the thoracic spine, but no other abnormalities. Her laboratory findings included a normocytic, normochromic anemia; Bence-Jones proteinuria; and a monoclonal spike in the gamma-globulin region on serum protein electrophoresis (SPEP).
Radiographic Findings
Lateral (Figure 1) and anterior-posterior (AP) (Figure 2) radiographs displayed multiple sharply defined, round, punched-out, lucent foci throughout the woman’s skull, cervical spine, and mandible. However, the lesions did not appear to have a sclerotic border, and the foci spared the inner table of bone.

Figure 1
This lateral radiograph of the skull displays many punched-out, sharply defined, lytic defects throughout the skull, as well as the cervical spine and mandible. The lesions do not seem to have a sclerotic border, and the foci spare the inner table of bone.
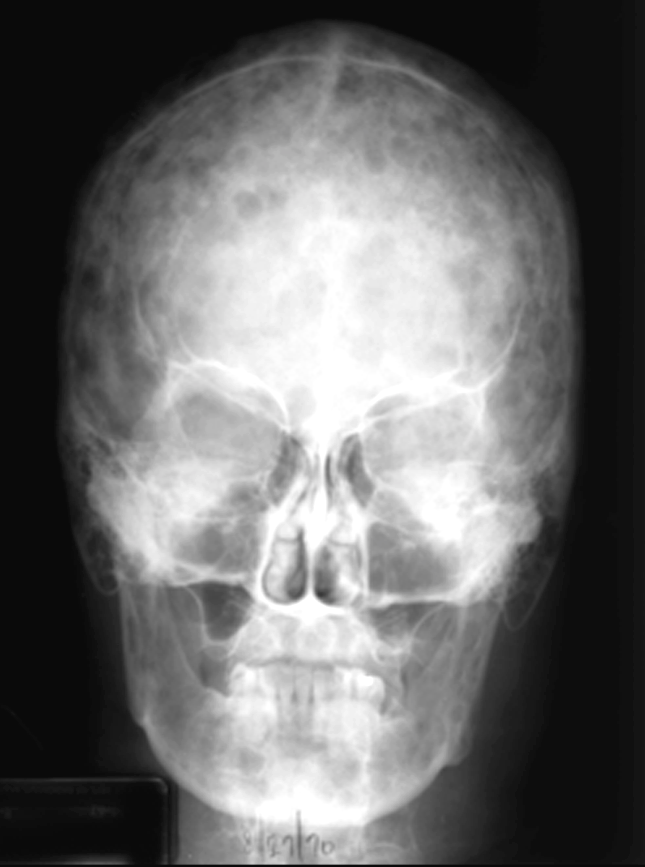
This AP skull radiograph cross-references Figure 1 to display the multiple lytic defects throughout the skull and mandible.
Figure 2
The lumbar spine films (not shown) displayed extensive demineralization and severe compression fractures at the 10th and 11th thoracic verterbrae and the 4th lumbar vertebra. A posterior-anterior (PA) chest radiograph (not shown) confirmed rib fractures, lytic bone defects, a questionable infiltrate in the lower region of the left lung, and kyphosis of the thoracic spine.
The AP pelvis radiograph (Figure 3) displayed multiple variable, sharply defined lytic areas and Ethiodol contrast enhancement from a lymphangiogram in the right inguinal lymph nodes.

Figure 3 This AP pelvic radiograph displays multiple lytic areas and Ethiodol contrast material from a lymphangiogram in the right inguinal lymph nodes (arrows). Observe the endosteal scalloping of lucent areas within the femurs (bar arrow).
Diagnosis
The differential diagnosis included round cell tumors of the bone, especially multiple myeloma and lymphoma. As the skull findings were classic for myeloma, the diagnosis was multiple myeloma. Postmortem evaluation disclosed malignant reticuloendotheliosis, mild myocardial and pulmonary calcinosis, nephrocalcinosis, amyloid infiltration of the small bowel, and pericardial effusion.
Discussion
Multiple myeloma is a malignant round cell tumor of bone that contains a neoplastic proliferation of plasma cells. However, it is a relatively uncommon cancer.
In the United States, the lifetime risk of multiple myeloma is one in 149 (0.67%). The American Cancer Society (ACS) has estimated that approximately 24,050 new diagnoses of multiple myeloma will be made in 2014, with about 11,090 related deaths expected to occur this year.
Some clinicians consider myeloma to be the most common primary bone lesion. Although its incidence is rare among those aged younger than 40, risk for myeloma increases with age, resulting in a median age at presentation in the mid-60s.
Bony signs and symptoms vary from localized pain and tenderness to fractures. They particularly involve bones in the spinal column, though some patients are asymptomatic and the myeloma is found incidentally. Pain, which is the most common symptom, is reported by 70% of patients.1 Recurrent bacterial infections are a presenting feature in about one-fourth of myeloma patients, and another three-fourths will suffer a serious infection during the course of the disease.1
Other conditions associated with multiple myeloma include anemia; hypercalcemia, which can lead to renal disease and even renal failure; and neurologic symptoms, such as weakness, confusion, and hyperviscosity.1 On plain radiographs, the lesions may appear solitary, generalized, or multiple. Since the lesions are lytic and seldom associated with new osteoclastic bone formation, plain radiography is more useful as a diagnostic tool than radioisotopic bone scans. Laboratory findings may include Bence-Jones protein in the urine, anemia, abnormal renal function results, and a monoclonal spike in the globulin fraction on SPEP.
Treatment of multiple myeloma has improved significantly over the past few decades and generally includes systemic chemotherapy to slow myeloma progression, in addition to supportive care against its complications, such as bisphosphonates to reduce skeletal problems.1
Imaging tests can also help doctors make a diagnosis of multiple myeloma and measure its spread. Plain X-ray films of the body's large bones taken in a skeletal bone survey may identify an impeding pathologic fracture.2 In a few patients, magnetic resonance imaging (MRI) or positron emission tomography (PET) may be necessary to find bone involvement from multiple myeloma.
Take-home Message
When a patient’s presenting complaint is chest pain, consider plain radiographs directed to the area of pain and do not forget to look at the bones. In plain radiographs with multiple lytic, bony lesions, contemplate round cell tumors of bone, particularly multiple myeloma and lymphoma. The lytic, punched-out lesions, as well as expansile rib lesions, are typical of myeloma.2 Impeding patholytic fractures may be best detected by multiplane MRI.
References
1. Munshi NC, Longo DL, Anderson KC. (2005). Plasma cell disorders. Harrison's Principles of Internal Medicine. (16th ed.). New York: McGraw-Hill.
2. Meschan I. (1976). Synopsis of Analysis of Roentgen Signs in General Radiology. Saunders.
About the Author
James D. Collins, MD, is Professor and General Radiologist in the Department of Radiology at the UCLA David Geffen School Medicine. He formerly served as Director of the required medical student training for the department and President of the James T. Case Radiologic Foundation. Collins has an extensive background of publications, consultations, and editorial positions, including his current post as the Radiology Editor for the Journal of the National Medical Association. He specializes in bilateral 3-dimensional MRI and MRA imaging of the brachial plexus and has been performing those studies since 1985.






