Publication
Article
Targeted Therapies: Hepatitis C
Updated Guidelines Help Prioritize Treatments in Hepatitis C
Author(s):
Treatment for hepatitis C should be offered to the sickest patients first, according to updated guidelines from the Infectious Diseases Society of America and the American Association for the Study of Liver Diseases.
Treatment for hepatitis C should be offered to the sickest patients first, according to updated guidelines from the Infectious Diseases Society of America and the American Association for the Study of Liver Diseases.1,2
Because chronic hepatitis C virus (HCV) infection is a disease that may remain latent for many years, prioritizing treatment is a reasonable strategy. Many patients experience a smoldering infection that gradually worsens and leads to life-threatening consequences after 20 to 30 years.3
According to Donald M. Jensen, MD, director of the Center for Liver Diseases at the University of Chicago Medical Center, “We can’t treat all 3 million to 4 million patients immediately, so there has to be some way of prioritizing treatment.”1
Although the guidelines do not refer directly to the high cost of HCV regimens, Jensen notes, “Societal resources may limit the feasibility of treating all patients within a short period of time.”2
Guideline Recommendations
According to the guidelines (Table), patients who should receive the highest priority for treatment are: (1) those with advanced fibrosis or compensated cirrhosis, indicated by a METAVIR fibrosis score of F3 or F4; (2) those who have had a liver transplant; and (3) those with severe extrahepatic complications, including1,2:
- Proteinuria
- Nephrotic syndrome
- Membranoproliferative glomerulonephritis, or essential mixed cryoglobulinemia type 2 or type 3 with end-organ damage, such as kidney damage or vasculitis (approximately 10%-15% of patients with chronic HCV infection have vasculitis related to cryoglobulinemia)4
After the highest priority patients, the guidelines recommend earlier treatment for patients with comorbidities that increase the risk of serious HCV complications. These comorbidities include1,2:
- HIV-1 infection
- Hepatitis B infection
- Porphyria cutanea tarda
- Type 2 diabetes mellitus
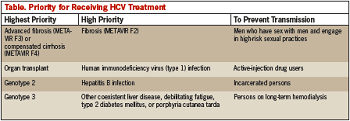
Another category of patients who should receive early treatment are those likely to transmit HCV to another person. These include men who have sex with men, active-injection drug users, and prisoners. Patients on long-term hemodialysis should also receive early treatment to prevent further transmission. Of the 8% to 9% of patients on hemodialysis who have HCV infection, most are thought to have acquired the infection nosocomially through contaminated hemodialysis equipment.2,5
Finally, certain patients may be at higher risk of fibrosis progression, which may be a consideration in deciding when to initiate therapy. The guidelines note that fibrosis may progress more rapidly in patients with genotype 3 HCV infection and in patients who smoke, although the presence of these risk factors does not place patients in high-priority treatment groups.1,6,7
The Benefits of Prioritizing Therapy
The annual incidence of cirrhosis in patients with HCV infection is approximately 3.9%,2,8 and each year approximately 7.5% of patients with hepatitis C will experience death, hepatic decompensation, hepatocellular carcinoma, or advancing Child-Pugh scores.2,9
Fortunately, curative HCV treatment can slow or reverse HCV-related damage. With therapy, patients who achieve a sustained viral response (SVR) can experience improvements in liver histology and reductions in the rate of liver fibrosis progression. Cirrhosis resolves in approximately half of cases of treatment-naïve patients with HCV-related cirrhosis who experience an SVR.10
In addition, with each SVR, the risk of hepatocellular carcinoma falls by 70%, and the likelihood of requiring a transplant or dying from liver disease falls by a factor of 10.2,11
SVR attainment may also lead to remissions of lymphoproliferative disorders, including non-Hodgkin lymphoma, and lower rates of mortality from cryoglobulinemia-related vasculitis.2
With interferon-free therapies, SVR rates are expected to improve. The costs of treatment may also fall with near-term approval of 3 interferon-free, ribavirin-free combination tablets for hepatitis C.
“We also know that treatments and therapies will improve over time, and as those therapies improve it may even be better for some of those people who can wait,” Jensen stated.1
References
1. McCarthy M. Treat sickest hepatitis C patients first, new US guidelines recommend. BMJ. 2014;14;349:g5163.
2. AASLD/IDSA. AASLD/IDSA Guidelines for Treatment of Hepatitis C. http://www.hcvguidelines.org/full-report/whenand-whom-initiate-hcv-therapy. Accessed August 2014.
3. World Health Organization. Hepatitis C fact sheet. http://www.who.int/mediacentre/factsheets/fs164/en/. Accessed August 2014.
4. Fabrizi F, Dixit V, Messa P. Antiviral therapy of symptomatic HCV-associated mixed cryoglobulinemia: meta-analysis of clinical studies. J Med Virol. 2013;85(6):1019-1027.
5. Centers for Disease Control and Prevention. Recommendations for preventing transmission of infections among chronic hemodialysis patients. MMWR Recomm Rep. 2001;50(RR-5):1-43.
6. Kanwal F, Kramer JR, Ilyas J, Duan Z, El-Serag HB. HCV genotype 3 is associated with an increased risk of cirrhosis and hepatocellular cancer in a national sample of U.S. Veterans with HCV. Hepatology. 2014;60(1):98-105.
7. Konerman MA, Mehta SH, Sutcliffe CG, et al. Fibrosis progression in human immunodeficiency virus/hepatitis C virus coinfected adults: prospective analysis of 435 liver biopsy pairs. Hepatology. 2014;59(3):767-775.
8. Sangiovanni A, Prati GM, Fasani P, et al. The natural history of compensated cirrhosis due to hepatitis C virus: a 17-year cohort study of 214 patients. Hepatology. 2006;43(6):1303-1310.
9. Everson GT, Hoefs JC, Seeff LB, et al. Impact of disease severity on outcome of antiviral therapy for chronic hepatitis C: Lessons from the HALT-C trial. Hepatology. 2006;44(6):1675-1684.
10. Poynard T, McHutchison J, Manns M, et al. Impact of pegylated interferon alfa-2b and ribavirin on liver fibrosis in patients with chronic hepatitis C. Gastroenterology. 2002;122(5):1303-1313.
11. Morgan RL, Baack B, Smith BD, Yartel A, Pitasi M, Falck-Ytter Y. Eradication of hepatitis C virus infection and the development of hepatocellular carcinoma: a meta-analysis of observational studies. Ann Intern Med. 2013;158 (5,p+1):329-337.






