Article
Gut Microbe Plays Major Role in Macular Degeneration
Author(s):
Age-related macular degeneration, the leading cause of blindness in the developed world, has long been linked to diet and obesity. Recently, we came closer to understanding just exactly why that is.
As with so many other health concerns, the leading cause of blindness in the developed world may originate in the gut.
A team from the University of Montreal led by Elisabeth MMA Andriessen recently sought to examine how the bacterial composition of the intestines may influence the risk of age-related macular degeneration in its neovascular form (nvAMD). Fat deposits in the eye, called drusen, are associated with early AMD. “Wet” AMD, the disease in its late stage, is marked by choroidal neovascularization (CNV), the formation and, occasionally, rupturing of new and fragile blood vessels in the eye. The leakage is referred to as exudate, and wet AMD is interchangeably referred to as “exudative AMD.”
According to the American Academy of Ophthalmology, obesity is among the five most common factors in the development of AMD. A press release that accompanies the new University of Montreal study says that “in men, overall abdominal obesity is the second most important environmental risk factor, after smoking, for progression to late-stage blinding AMD.” To date, the mechanism behind that remained unknown.
For the research, two sets of mice were raised on two different diets from 6 weeks old: a regularâ€chow diet (RD; 16% kcal fat) or a highâ€fat diet (HFD; 60% kcal fat). Expectedly, the HFD mice gained 50% more weight. They examined the composition of their gut microbiomes. “Bacteroidetes/ Firmicutes ratios shifted from 66%/33% of total bacteria in RD to 19%/67% in HFD,” the authors write. Bacteroidetes are typically the dominant of those two most common phyla in the guts of lean individuals. The study notes that HFD mice had more diverse gut flora, with “modest but important presence of Actinobacteria and Spirochaetes” which were not apparent in the guts of the RD mice.
Some of the HFD mice were treated with neomycin, which was uncoupled from physical weight gain but worked to restore the Bacteroidetes/Firmicutes ratio in the gut to one more consistent with the RD mice. Those treated HFD mice showed comparable levels of CNV to the RD mice, whereas the untreated HFD mice previously showed “a robust 60% increase in CNV in HFDâ€fed mice when compared to RD controls” in earlier confocal imaging following a laser burn to the eye. As such, the authors were able to associate gut dysbiosis with CNV.
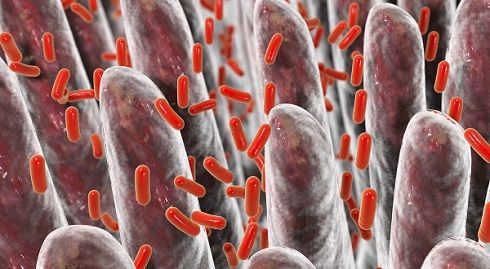
Further exploring the mechanism, they observed differences in the expression of mononuclear phagocytes (MPs) such as microglia and macrophages between the mice with different gut flora. “The heightened CNV observed in HFDâ€fed mice…was accompanied by a ~twofold increase in MPs and microglia at sites of lesion when compared to control RDâ€fed mice,” persisting 14 days after the burn, according to the researchers, bringing them to the conclusion that “the intestinal microbiota of HFDâ€fed mice augments recruitment of microglia and other MPs that may be central to disease progression.” They also determined that the flora of the HFD mice allowed for furthers systemic inflammation.
Testing their findings, they performed fecal transplants across the two dietary groups, finding that “transfer of RD microbiota to HFDâ€fed mice diminished CNV by ~35% supporting a role for gut microbiota in pathological CNV” and noted the transplants resulted in reduced overall inflammation for the HFD mice.
In an unaffiliated commentary on the study published alongside it in EMBO Molecular Medicine, Rebecca Scholz and Thomas Langmann underscore the findings: “The experiments by Andriessen et al (2016) in this issue…demonstrate that “obese microbiota” can challenge the retinal innate immune system to drive pathological angiogenesis,” later saying that the Montreal researchers “provide a novel link between homeostasis of gut microbiota and ocular angiogenesis mediated via systemic and local immune processes.”
As both obesity rates and life expectancies continue to balloon, this work may be of great importance in slowing the progression of AMD and avoiding the blindness that it often brings.
The original article, entitled “Gut microbiota influences pathological angiogenesis in obesityâ€driven choroidal neovascularization,” was published in November in EMBO Molecular Medicine, alongside the commentary “Gut flora connects obesity with pathological angiogenesis in the eye.” The University of Montreal issued an accompanying press release upon its publication.
Related Coverage:
Mediterranean Diet May Deter Macular Degeneration
Researchers Close In on Genetics of Age-Related Macular Degeneration
Genetic Mutation Responsible for Form of Macular Degeneration



