Publication
Article
Internal Medicine World Report
Glucosamine Supplement Fails to Slow Joint Deterioration in Chronic Knee Pain Trial
Author(s):
Although it is believed to help counteract joint and cartilage deterioration in osteoarthritis (OA), glucosamine supplementation is no more effective than placebo in preventing knee degeneration in patients with chronic knee pain.

Although it is believed to help counteract joint and cartilage deterioration in osteoarthritis (OA), glucosamine supplementation is no more effective than placebo in preventing knee degeneration in patients with chronic knee pain, according to a study published in the April 2014 issue of Arthritis & Rheumatology.
For their randomized, double-blind, placebo-controlled trial, C. Kent Kwoh, MD, Director of Clinical Research in the Division of Rheumatology and Clinical Immunology at the University of Pittsburgh and Chief of the Rheumatology Section at the VA Pittsburgh Healthcare System, and his colleagues randomized 201 participants aged 35-65 years with typical symptoms of knee OA to receive either placebo or 1,500 mg of Cargill’s oral Regenasure glucosamine hydrocholride supplement for 24 weeks.
Noting the plain radiographs used in previous glucosamine efficacy studies “are an indirect, insensitive measure of structural progression in OA,” the researchers utilized 3 Tesla magnetic resonance imaging (3T MRI) of both knees and urinary C-terminal crosslinking telopeptide of type II collagen (CTX-II) excretion — high levels of which indicate cartilage tissue loss — to monitor the participants’ disease progression and assess the benefits of the supplementation.
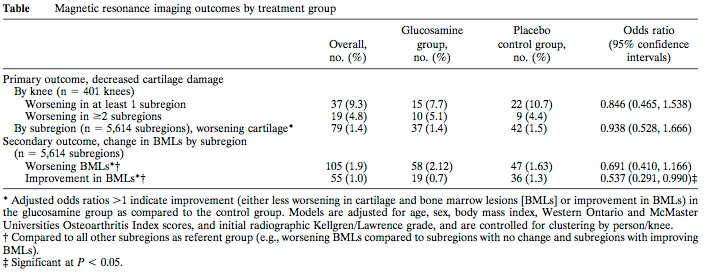
On the primary outcome measure of decreased cartilage deterioration in each knee, “there was no statistically significant difference in cartilage worsening between the glucosamine group and the control group” at the 24-week mark compared to baseline 3T MRI measurements, Kwoh and his co-authors reported. Additionally, the investigators found no meaningful differences in worsening bone marrow lesions (BMLs), reduced knee pain, or improved knee function between the 2 study populations at the trial’s conclusion.
Remarkably, the control participants exhibited more improvement in BMLs than those who received the supplementation, and “the excretion of urinary CTX-II was decreased in the control group compared to the glucosamine group,” the authors wrote. As a result, the researchers were “unable to demonstrate a benefit of glucosamine over placebo with regard to improvement in BMLs” and decreased CTX-II excretion.
In response to all of their reported findings, Kwoh and his colleagues concluded they “did not find any evidence that glucosamine is more effective than placebo in improving joint health” in patients with chronic knee pain over a 24-week period.






