Article
AHA/ASA Release Updated Guidelines for Secondary Prevention After Stroke or TIA
Author(s):
The American Heart Association and American Stroke Association have released an updated version of their guidelines for prevention of secondary stroke in patients with stroke or TIA, which had not been updated since 2014.
The American Heart Association and American Stroke Association have released new clinical practice guidelines aimed at reducing secondary stroke risk in patients with stroke or transient ischemic attack (TIA).
Endorsed by the American Association of Neurological Surgeons, Congress of Neurological Surgeons, and the Society of Vascular and Interventional Neurology, the 104-page guideline update addresses secondary prevention in this patient population in 4 sections: diagnostic evaluation, vascular risk factor management, management by etiology, and systems of care for secondary prevention of ischemic stroke. An accompanying data review article was published simultaneously, outlining the current available evidence related to short-term and long-term dual versus single antiplatelet therapy.
“It is critically important to understand the best ways to prevent another stroke once someone has had a stroke or a TIA,” said Dawn O. Kleindorfer, MD, FAHA, chair of the guideline writing group, and professor and chair of the department of neurology at the University of Michigan School of Medicine, in a statement from the AHA. “If we can pinpoint the cause of the first stroke or TIA, we can tailor strategies to prevent a second stroke.”
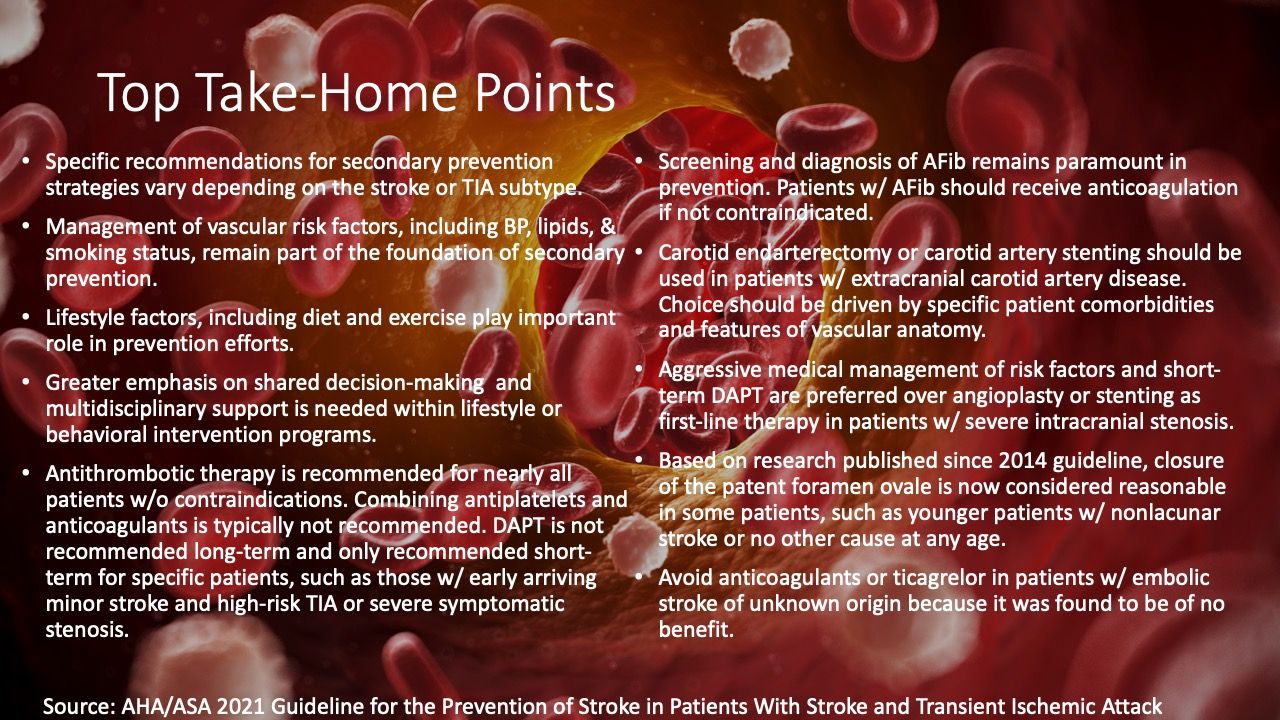
This latest guideline update, which is the first to address secondary prevention of stroke in this population since the ASA’s 2014 guidelines, was designed to provide updated evidence-based recommendations and relay information in a manner that is more accessible for clinicians. Atop the guidelines is a list of the top 10 take-home messages from within the guideline.
The accompanying systematic review detailed a systematic review and meta-analysis performed on behalf of the AHA Stroke Council detailing relevant data comparing dual versus single antiplatelet therapy for secondary stroke prevention. After a search of multiple databases from 1999-2019, investigators identified 3 short-duration randomized controlled trials and 2 long-duration treatment randomized controlled trials for inclusion in the meta-analyses.
Upon analysis, DAPT was associated with a lower 90-day risk of recurrent ischemic stroke (pooled RR, 0.68; 95% CI, 0.55–0.83; I2=37.1%) than single antiplatelet therapy. Investigators also pointed out there was no increase in major bleeding observed with DAPT in short-duration trials (pooled RR, 1.88; 95% CI, 0.93-3.83; I2=8.9%).
When examining data from a pair of long-duration randomized clinical trials (mean duration 18-40 months), DAPT was not associated with a significant reduction in recurrent ischemic stroke (pooled RR, 0.89; 95% CI, 0.79-1.02; I2=8.9%) and was also associated with increased risk of major bleeding (pooled RR, 2.42; 95% CI, 1.37-4.30; I2=75.5%).
This statement, “2021 Guideline for the Prevention of Stroke in Patients With Stroke and Transient Ischemic Attack: A Guideline From the American Heart Association/American Stroke Association,”, and accompanying review article, titled “Benefits and Risks of Dual Versus Single Antiplatelet Therapy for Secondary Stroke Prevention: A Systematic Review for the 2021 Guideline for the Prevention of Stroke in Patients With Stroke and Transient Ischemic Attack,”, were published in Stroke.





