Article
Bone Infarcts in Systemic Lupus Erythematosus
A 45-year-old woman presented with longstanding left knee pain. Both knee and hand radiographs showed abnormalities. Bony infarcts had become complicated by an infection/septic joint and had progressed to frank bony destruction.
A 45-year-old woman presented with longstanding left knee pain. Radiographs (below) were obtained on February 18 (left) and September 5 (right).

FINDINGS: In the radiographs above, the one taken on 2/18 (left) shows subtle densities that are more conspicuous on the radiographs of 9/5 (right). These densities have a serpiginous, well defined, sclerotic border. A lateral image taken on 9/5 appears at left below.
Hand radiographs (below, right) demonstrate ulnar subluxation of the metacarpophalangeal joints, but without erosive changes.


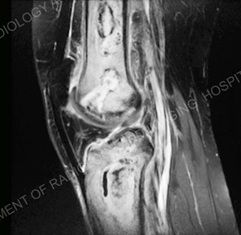
An MRI (below, left) demonstrates well demarcated, serpiginous areas with surrounding high and low signal borders. This corresponds to the foci of bone infarct. Atypical is the vast high signal seen within the femur and tibia. A CT image (below, right) demonstrates central sclerotic foci of bone necrosis with large areas of surrounding lucency and cortical destruction of the anterior tibia.

Click here to read the Discussion and Resolution of the case..
DISCUSSION: Bone infarcts are seen in a multitude of conditions, predominantly at our institution from previous trauma, steroid use, and in the setting of a vasculitis.
Infarcts associated with systemic lupus erythematosus (SLE) are thought to be in part secondary to steroid treatment but also secondary to the underlying vasculitis that afflicts multiple organ systems in these patients.
The nonerosive subluxation or Jacoud-type arthropathy of the hand is classic for SLE, and helps in narrowing the differential of a bone infarct.
RESOLUTION: The infarcts in this patient had become complicated by an infection/septic joint and had progressed to frank bony destruction. High signal in the femur and tibia on the MRI was either secondary to the infection itself or a manifestation of an inflammatory response
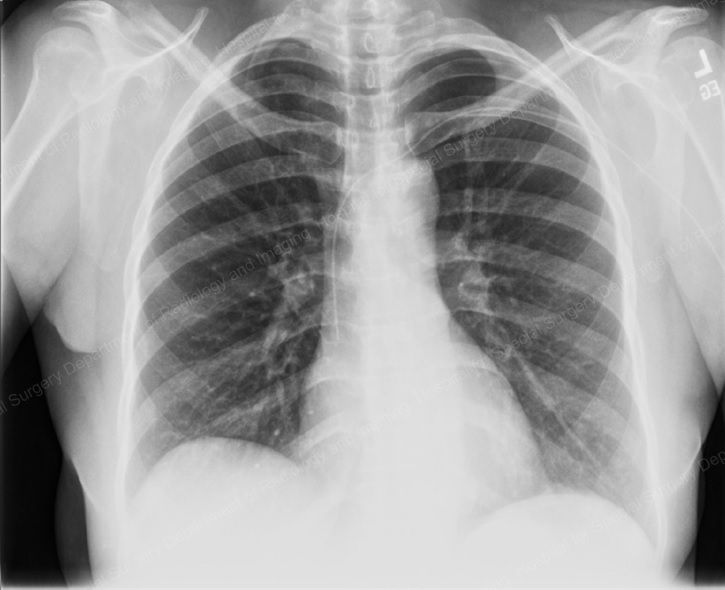

A peripheral Intravenous central catheter was placed to administer IV antibiotics (above, left) and antibiotic infused methylmethacrylate spacers were placed in the knee to treat the infection (right).
References:
RESOURCES
Resnick. Bone and Joint Disorders 4th edition. 2002
http://www.cmaj.ca/cgi/content/full/174/4/455
Cervera R, Piette JC, Font J, et al. Antiphospholipid syndrome: clinical and immunologic manifestations and patterns of disease expression in a cohort of 1,000 patients. Arthritis Rheum 2002;46:1019-27.




