Article
Pseudoseptic Arthritis Secondary to Calcium Pyrophosphate Disease
When all signs point to septic arthritis, microcrystalline arthritis may be at fault. These authors anticipated ordering antibiotics and orthopedic consultation, but found a very simple solution for their patient with disabling knee effusion.
A 75-year-old Filipino man presented to the ambulatory medicine clinic with two days of atraumatic right knee swelling and loss of motion. He had returned from the Philippines one week previously. He denied any constitutional symptoms such as fevers, chills, or night sweats.
His pertinent past medical history was significant only for osteoarthritis. He had become wheelchair- bound, and his examination revealed an asymmetric right knee effusion. There was obvious erythema that was warm to the touch. Crepitus was elicited bilaterally. Passive and active range of motion in his right knee were limited, and it was tender to palpation.
Our differential diagnosis included septic arthritis, crystalline arthropathy (namely, gout and pseudogout), reactive arthritis, and gonococcal infection.
Clinical Findings
Joint aspiration produced grossly milky white pus with some blood streaking due to a mildly traumatic tap. Cell count was 112 cells/mcL, 103 red blood cells (RBC)/mcL, 18%
polymorphonuclear neutrophils(PMNs), 43% lymphocytes, and 36% monocytes. Gram stain and culture were negative. HIV antibody and chlamydial/gonococcal urine DNA probes were negative.
We deferred ordering C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), and the procalcitonin test (PCT), because the physical exam was overwhelmingly characteristic of an inflammatory process. Because the patient denied any traumatic event and we strongly suspected septic arthritis, we did not order any plain films, but elected to aspirate the joint for definitive diagnosis.
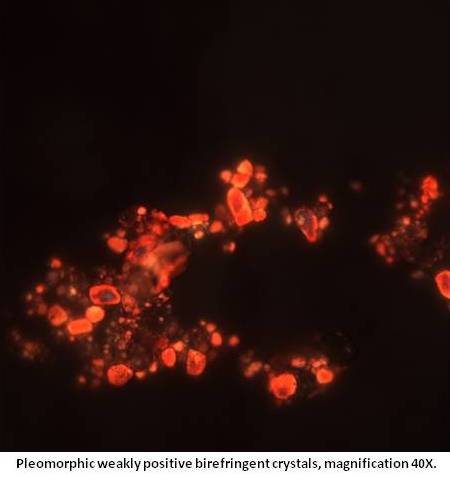
We identified numerous weakly positive birefringent pleomorphic crystals (see image at left) but we saw no monosodium urate crystals.
Diagnosis
We made the diagnosis of pseudoseptic arthritis secondary to calcium pyrophosphate deposition disease, given patient’s clinical presentation of septic arthritis with identified weakly positive birefringent pleomorphic crystals on joint aspirate.
In our patient, pseudogout was the underlying disease, mimicking septic arthritis. Our patient’s clinical presentation was so convincing that we deferred the typical inflammatory diagnostic evaluation (CRP, ESR, PCT, plain films) for definitive diagnostic joint aspiration, anticipating the need for urgent antibiotic treatment and orthopedic consultation.
Instead, in light of the imaging evidence, we were able to resolve the problem by completely draining the patient’s knee. Returning to our clinic four days later, he had complete resolution of symptoms without any pharmacologic intervention. He was bearing weight without restriction and was ambulating free of assistive devices. Motion was restored and the effusion was resolved.
Discussion
The term pseudoseptic arthritis is used to describe a clinically expressive septic joint and a purulent aspirate when no microorganisms can be isolated. Several inflammatory conditions may cause pseudoseptic arthritis, among them microcrystalline arthritis which includes gout, pseudogout, and hydroxyapatite or oxalate deposition.
The incidence of pseudoseptic arthritis is largely unknown. Singleton et al reported 6 cases of pseudoseptic arthritis (1.8%) in a series of 328 patients with rheumatoid arthritis who underwent arthrocentesis.1 More recently, Eberst-Ledoux et al reported that in 74 of 398 patients with presumed septic arthritis (19%), no microorganism was isolated from synovial fluid or blood samples.2
Suspicion for septic arthritis should remain high in this setting. However, once it has been ruled out, the possibility of microcrystalline arthritis and other inflammatory arthropathies should be explored.
(References appear beneath the Comments box below.)
References:
REFERENCES
1. Singleton JD, West SG, and Nordstrom DM
"Pseudoseptic" arthritis complicating rheumatoid arthritis: a report of six cases.
J Rheumatol
(1991) 18:1319-1322.
2. Eberst-Ledoux J, Tournadre A, Mathieu S
et al.
Septic arthritis with negative bacteriological findings in adult native joints: a retrospective study of 74 cases.
Joint Bone Spine
(2012) 79:156-159.




