Article
3-month HbA1c Predicts Success of GLP-1 RA Therapy
Author(s):
Not all patients with type 2 diabetes respond equally to GLP-1 receptor agonists. Results of a recent study suggest what to look for before you write that next Rx.
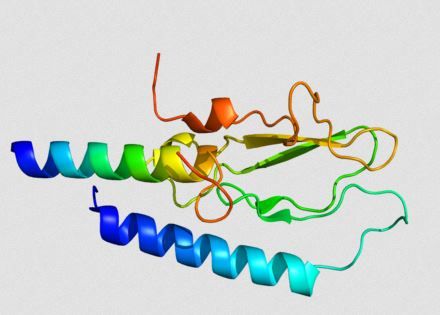
GLP-1 receptor
Patients with type 2 diabetes (T2DM) who show significant reductions in HbA1c (A1c) within 3 months of starting treatment with the glucagon-like peptide-1 (GLP-1) receptor agonist exenatide were more likely to also be responders by 6 months, according to the results of a retrospective analysis published in theJournal of Diabetes Research.
According to the study, although research has shown that GLP-1 analogues effectively reduce A1c and weight in patients with T2DM, groups of patients still fail on treatment for 2 primary reasons: intolerable adverse events or failure to achieve the treatment goal.
“Within the UK, NICE [the National Institute of Health and Care Excellence] defines an individual who is said to have ‘responded’ to therapy if their baseline weight and glycated haemoglobin (HbA1c) have reduced by 3% and 11 mmol/mol (1%), respectively, after six months of GLP-1 analogue administration,” wrote researchers led by Muhammad Khan, of Countess of Chester Hospital NHS Foundation Trust, United Kingdom. In cases where these goals are not met, patients are often recommended to move on to another therapy, often insulin.
In this analysis, Khan and colleagues wanted to explore factors that might characterize which patients respond to treatment with GLP-1 analogues and which do not. The ability to identify early in treatment individuals unlikely to respond to GLP-1 analogues would eliminate the potential risk of exposure to a 6-month period of side effects as well as the expense associated with GLP-1 analogues without any clinical benefit. That class of drugs being eliminated, the next most suitable therapy for the patient and stage of disease can be initiated.
Exenatide was selected for the study GLP-1 receptor agonist as it has the longest record of clinical use.
The study included 112 patients initiated on exenatide between 2008 and 2014 for who there was information available on age, gender, duration of diabetes, concurrent diabetes medications, weight, body mass index, and A1c at baseline (date of exenatide initiation), 3 months, and 6 months.
The researchers identified 63 patients as responders, with an 11 mmol/mol reduction in A1c at 6 months, and 49 patients as nonresponders.
No significant difference was found between responders and nonresponders for gender, age, or duration of diabetes. However, the researchers did find that the group of nonresponders had significantly more participants on exenatide with insulin compared with the group of responders (20.4% vs. 3.17%; P=.0047).
The entire cohort of patients had significant reductions for weight and body mass index from baseline at 3 and 6 months, and both responders and nonresponders had significant reductions from baseline to 6 months (P<.0001).
In addition, the mean baseline A1c of 80.9 mmol/mol for the entire cohort was reduced to 70.4 mmol/mol by 3 months and to 67.8 mmol/mol by 6 months (P<.0001). However, data showed that change in A1c from baseline, 3 months and 6 months was the only significant difference between responders and nonresponders.
Patients identified as responders had a reduction in A1c from a baseline level of 85.1 mmol/mol to 67.8 mmol/mol at 3 months and 60.7 mmol/mol at 6 months (P<.0001). Regression analyses identified a negative linear relationship with higher baseline A1c correlating to greater reductions in HbA1c by 6 months (P<.0001).
“However, nonresponders demonstrated an initial reduction in A1c by 3 months (73.7 ± 12.9 mmol/mol) from baseline (75.5 ± 11.4 mmol/mol), yet by 6 months the A1c had risen to a level greater than baseline (77 ± 13.2 mmol/mol),” the researchers wrote.
Those patients with an A1c reduction of 15% to 20% or greater by 3 months were more likely to respond to exenatide by 6 months than those patients with lower reduction (P=.033).
“Our study provides a novel insight into the possibility of using the percentage change in A1c observed at 3 months of treatment to predict response by 6 months,” the researchers wrote. “We hope that our findings reinvigorate this field of research as with supplementary research we can ultimately develop a predictive model which both outlines and quantifies a series of predictor variables and changes allowing clinicians to identify, with a significant degree of confidence, individuals likely to respond to exenatide therapy.”
References:
Khan M, Ouyang J, Perkins K et al. Determining predictor of early response to exenatide in patients with type 2 diabetes mellitus.J Diabetes Res. 2015;2015:162718. Epub 2015 Jan 20.




