Article
A 45-Year-Old Woman With Acute Thumb Pain
A 45-year-old woman presented to the emergency department with a 3-day history of an acutely painful, swollen, and erythematous thumb. Ordinary x-ray was central to the correct diagnosis.
Given the clinical scenario, the aspiration results, and the radiographic findings, a diagnosis of acute calcific periarthritis (ACP) was determined. ACP is a self-limited condition caused by the deposition of hydroxyapatite (HA) crystals in tendons, bursae, and soft tissue spaces surrounding a joint.1 Once the HA crystals are deposited, an intense inflammatory reaction is triggered, causing the clinical condition of an acute monarthritis in a patient who does not have any overt trauma or other systemic symptoms.2

ACP affects the shoulder most frequently, followed by the hip, knee, elbow, wrist, and ankle joints; polyarticular cases are rare.3 This syndrome usually occurs between age 40 and 70 years; it affects men and women at equal rates.1 However, ACP of the hands and feet affects women much more frequently than men (ratio, 5:1), particularly women in the premenopausal age-group.4-6
In patients with ACP, the swelling, pain, and erythema develop rapidly over a course of hours to days. The joint may be tender to the touch, and range of motion is nearly always limited. Even in the absence of a particular intervention, the pain and swelling typically begin to improve after 1 week and resolve within 3 or 4 weeks. Relapse of this disease process is uncommon.1
No laboratory test is particularly helpful in making the diagnosis of ACP, including measures of calcium homeostasis, although white blood cell count may be reassuringly normal when infection is a consideration. Aspiration typically is sterile and without marked cellularity, although concomitant infection always is a possibility. HA crystals are difficult to visualize with conventional light microscopy because of their size (0.1 to 0.2 μm); alizarin red S stain may be used to screen an aspirate for the presence of calcium phosphate salts.1,7
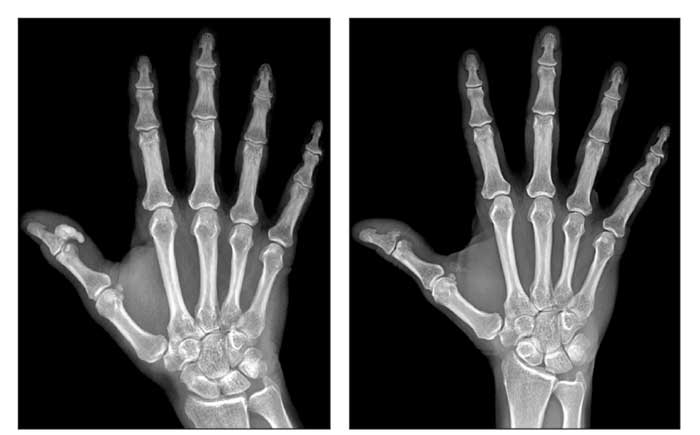
The key to making the diagnosis is plain radiography. X-ray films (below) demonstrate a dense, amorphous, homogeneous material at the site of involvement without cortex or internal trabeculations, the morphology of which may change over time. After an acute attack, there generally is a significant reduction in calcific density, often with near-complete resolution. It has been postulated that the intense inflammatory infiltrate may dissolve the calcified tissue.8
The treatment of choice for patients with ACP is full-dose NSAIDs, which also may help shorten the duration of the attack.9 Corticosteroids (oral and intra-articular) and colchicine have been used as alternative treatments.6 Additional conservative measures, such as splinting, may be beneficial.
The initial differential diagnosis typically includes pyogenic tenosynovitis, traumatic injury, septic arthritis, gout, pseudogout, tendinitis, cellulitis, and early inflammatory arthritis. Diagnosis often is delayed because the presentation of ACP may be indistinguishable from that of gout, pseudogout, or septic arthritis, underscoring the importance of combining the clinical scenario with radiography in patient evaluation.
The pathogenesis of the deposition of the HA crystals in the periarticular tissues is incompletely understood. Trauma, tendon degeneration, and local tissue hypoxia all are proposed as mechanisms that predispose an area to calcification. Pinals and Short3 had proposed a systemic explanation when describing a series of patients with recurring, polyarticular episodes, but the vast majority of cases are self-limited, local, 1-time events in which no systemic process appears to have been involved.
This case
allows for a review of the differential diagnosis of an acute small-joint monarthritis and
the inability of clinicians to always differentiate among the potential causes on the basis of the appearance and physical examination of the joint. The case also demonstrates the utility of x-ray films in the diagnosis of ACP, as well as the natural history of such attacks, including dissolution of the calcified tissue by the elicited inflammatory reaction.
An NSAID was prescribed, and the patient was discharged from the ED. When seen in follow-up 3 weeks later, she had experienced complete resolution of her symptoms. A second radiograph obtained at the follow-up visit (initial radiograph at left and second radiograph at right) showed that the tissue calcification had largely resolved.
References:
1. Resnick D. Calcium hydroxyapatite crystal deposition disease. In: Resnick D, ed. Diagnosis of Bone and Joint Disorders. 4th ed. Philadelphia: WB Saunders; 2002:1619-1657.
2. Yosipovitch G, Yosipovitch Z. Acute calcific periarthritis of the hand and elbows in women: a study and review of the literature. J Rheumatol. 1993;20:1533-1538.
3. Pinals RS, Short CL. Calcific periarthritis involving multiple sites. Arthritis Rheum. 1965;8:462.
4. Arandas Fde S, Santos FA, de Souza SP, et al. Acute calcific periarthritis of the hand. J Clin Rheumatol. 2005;11:223-224.
5. Gálvez J, Linares LF, Villalón M, et al. Acute calcific periarthritis of the fingers. Rev Rhum Engl Ed. 1995;62:602-604.
6. Mines D, Abbuhl SB. Hydroxyapatite pseudopodagra in a young man: acute calcific periarthritis of the first metatarsophalangeal joint. Am J Emerg Med. 1996;14:180-182.
7. Paul H, Reginato AJ, Schumacher HR. Alizarin red S staining as a screening test to detect calcium compounds in synovial fluid. Arthritis Rheum. 1983;26:191-200.
8. Doumas C, Vazirani RM, Clifford PD, Owens P. Acute calcific periarthritis of the hand and wrist: a series and review of the literature. Emerg Radiol. 2007;14:199-203.
9. Fam AG, Rubenstein J. Hydroxyapatite pseudopodagra: a syndrome of young women. Arthritis Rheum. 1989;32:741-747.




