News
Article
60 Years of Progress: How the 1964 Surgeon General Report has Shaped Modern Healthcare
Author(s):
In this feature, we acknowledge the impact of the 1964 Surgeon General report, its subsequent effect on public health, and present-day hurdles to optimized public health efforts through the eyes of our editorial advisory board members and other leading experts.
Luther Terry, MD, displays the 387-page 1964 Surgeon General Report.
Credit: US Centers for Disease Control and Prevention
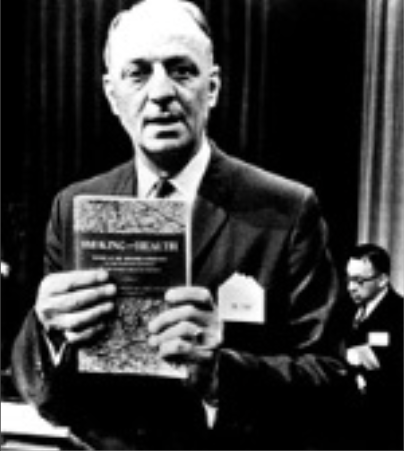
As he made his way to the podium to deliver his address on January 11, 1964, few could have imagined the historic significance of the document Luther Terry, MD, the 9th Surgeon General of the United States, would go on to capture in the landscape of public health and culture across the nation.
Titled Smoking and Health: Report of the Advisory Committee to the Surgeon General of the Public Health Service, the address represented the culmination of mounting evidence and a 14-month review carried out by 10 physicians and scientists, along with 150 consultants. At 387 pages in length, the report leveraged more than 7000 scientific articles to confirm the growing suspicions surrounding causal links between smoking and adverse health consequences that, today, are accepted as common knowledge.1
Among the key highlights from the report was evidence of a 70% increase in the mortality rate, a 9- to 10-fold increase in risk of developing lung cancer, and a dose-response association with coronary heart disease. The ensuing 60 years would feature countless research updates, initiatives, and societal reforms spurred by the information within this report that would forever alter the course of public health and culture.1
“This report alerted the nation, really for the first time, to the health risks of smoking and it transformed the issue from one of just individual and consumer choice to really one of epidemiology, public health, and risk for smokers and nonsmokers alike,” explained Albert Rizzo, MD, chief medical officer of the American Lung Association and HCPLive editorial advisory board member.
At the height of cigarette smoking in the US during the 1960s, 42% of US adults smoked and the average US adult smoked more than 4000 cigarettes per year. These figures have since careened and, as of 2021, the prevalence of cigarette smoking among US adults is fewer than 12%.2,3
The downstream effect of this decline on health can be seen in the 8.0 million lives saved from premature smoking-attributable deaths with tobacco control measures from 1964–2012. According to a study from Yale, the average 40-year-old man could expect to live nearly 8 years longer than he would have in 1964, with 30% of this benefit derived from tobacco control.4
However, despite this decline, the US Centers for Disease Control and Prevention regard smoking as the leading cause of the mortality, accounting for more than 480,000 deaths each year, or about 1 in 5 deaths. In this feature, we acknowledge the impact of this report, its subsequent effect on public health, and present-day hurdles to optimized public health efforts through the eyes of our editorial advisory board members, as well as leading experts.5
Pulmonology
The story of tobacco smoking trends in the US does not move in a straight line, historically speaking. In fact, though tobacco was available in centuries past, the story does not significantly begin until the early 20th century.
As a result of technological advances in the arenas of transportation, manufacturing, and communication, the early half of this century featured a dramatic upswing in prevalence of smoking among US adults. In fact, most of the country refrained from smoking for decades into the 1900s. In 1910, the number of cigarettes consumed by the average US adult was less than half of what it was in 2010.6
With a lack of regulatory control over advertising and extensive influence of the tobacco industry within government and popular culture, smoking eventually reached its peak of 42% of the adult population in 1965. While it may seem in hindsight as though Americans were completely in the dark about the dangers of smoking for lung health until the report came out, this view is somewhat erroneous.6
Throughout the first few decades of the 20th century, periodic debates were already taking place on the pulmonary health hazards of smoking as it continued to gain popularity among Americans. Even as early as the 1950s, the link between lung cancer deaths and smoking was becoming apparent, thanks to the work of epidemiologists and their implementation of long-term, case-control surveys.1,6
Pathologists and other scientists were able to identify a statistical link not only between lung cancer but also other conditions impacting the lungs such as emphysema and bronchitis. In fact, smoking’s causal relationship to the epidemic rise of lung cancer in this period was declared on June 12, 1957, by Leroy E. Burney, MD, MPH, the 8th Surgeon General, as the official position of the US Public Health Service.6
Donald J. Alcendor, PhD
Credit: Vanderbilt University Medical Center

“I think when you go back to the 1960s, it is very clear that smoking was a problem,” said Donald J. Alcendor, PhD, associate professor from the department of pathology microbiology and immunology at Vanderbilt University Medical Center. “ I mean, you had 42% of Americans smoking at the time and that's almost half of adults smoking. That became a problem. It became a problem before the 1964 release of the Surgeon General's report…And it was very clear that at the time, you would meet with a lot of pushback. You had a strong, what I call, tobacco lobby.”
Following a joint plea from leading health organizations by 1961, some of which were the American Cancer Society and the American Heart Association, President John F. Kennedy made the call to convene a national commission on smoking. The committee was led by Terry, who was still a smoker himself until late 1963, and, after assessing studies conducted on the topic, the groundbreaking report was released on January 11, 1964.1,7
“In 1957, it was very clear from experiments that they did in laboratories that smoking was a cause of cancer, lung cancer,” Alcendor noted. “But the idea is that they held off on putting warnings on cigarette packages. They held off on coming to the public with this information, in a way that was not very clear, meaning that they didn't want to buck the system, so to speak. It was after only pressure by the Surgeon General at that time, Luther Terry, to come out and make this declaration, in a way that only he could make at the time, being the doctor of the nation.”
Since peaking in 1965, the decline in smoking among US adults has coincided with declines in pulmonary illnesses. Much of this, as a result of the messaging following the 1964, with warnings on cigarette packaging and elsewhere becoming more detailed on harms and cigarette advertising on television becoming more infrequent and less glamorized. In the pulmonary space, it was clear that lung cancer, emphysema, and bronchitis were all heavily impacted by smoking habits among patients.1,6
Cardiology
Although smoking has since been linked to deleterious health effects on almost all organs, its apparent effects on cardiovascular health are superseded only by its aforementioned impact on pulmonary function. According to the annual heart disease and stroke statistics report from the American Heart Association, which is celebrating its 100-year anniversary as an organization in 2024, coronary heart disease remains the leading cause of death in the US, but the rate of mortality from coronary heart disease has undergone a pair of revolutions.8
These revolutions, one representing a skyrocketing rate and the other showcasing a gradual decline of cardiovascular disease, both occurred during the 20th century and can be linked to popularity of smoking and tobacco use across the US.8
Viet Le, DMSc, PA-C
Credit: AAPA

“Since we've been tracking cardiovascular deaths, it's been astounding how the velocity of rise into cardiovascular deaths had been in the early part of this past century,” commented Viet Le, DMSc, PA-C, associate professor of research and a preventive cardiology PA at Intermountain Health as well as a member of HCPLive’s editorial advisory board. “And, really, that can be directly attributable to smoking. It's quite fascinating, if not terribly, just scary when you look at the statistics.”
Since 1921, heart disease has remained the leading cause of death in the US. Similar to rates of smoking, deaths from heart disease in the US peaked during the 1960s and began a gradual descent to current rates. During this time, the US experienced a shift in trajectory of cardiovascular disease rates nearly mirroring the decline in smoking.8
By 1996, 621,000 fewer deaths occurred from coronary heart disease than would have been expected had the rate remained at its 1963 peak and, by 2019, the years of life lost due to premature mortality from smoking had declined by 46.4% relative to 1900.8
The lasting impression made by the 1964 Surgeon General report is showcased within ongoing initiatives from the AHA and other major professional organizations in cardiology, including Tobacco-Free Kids, CardioSmart, and Life’s Essential 8. Debuted in 2022, Life’s Essential 8 is a group of 8 lifestyle factors outlined by the AHA as the factors linked to having the most profound impact on life expectancy—the first item on the list: avoiding smoking.9
“Across the United States, this is still something we need to focus on, but I'm just amazed at one Surgeon General report and its effect nationally,” Le added.
Lasting Public Health Effect
As evidenced above, the report has left an indelible impact on the culture of the US and the priorities of public health measures. Now, the report and subsequent public health efforts serve as a roadmap for ongoing and forthcoming public health campaigns. What this living case study demonstrates most prominently is the exhaustive level of time, resources, and cooperation needed to combat an issue so deeply ingrained within a nation’s culture.
The 1964 report was widely publicized—Terry described it as having "hit the country like a bombshell” when recalling its impact 20 years later—and directly called out the impact of smoking on health, it took several more years of education and regulatory interventions before the full effects could be felt.1,6
Despite more than a decade of growing evidence leading up to the report and widespread coverage in its aftermath, the consequential impact was not seen for several years. In a 1966 poll, just 40% recognized smoking as a major cause of lung cancer and one-third remained uncertain. A testament to the influence of the industry within healthcare, a 1982 memo from a then-editor of JAMA urged the editorial staff to “exercise appropriate caution in our JAMA publications on tobacco and control of tobacco use, nuclear war, and abortion”.6
Albert Rizzo, MD
Credit: American Lung Association

“While the report proclaimed that cigarette smoking is a health hazard of sufficient importance, and that importance led to a lot of changes, it really didn't come up with appropriate remedies,” Rizzo noted. “It mentioned that we should add [remedies], but those remedies were not outlined. So, it really fell to public health organizations to become advocates to lawmakers.”
As highlighted by Rizzo, much of the progress has been the result of education and aggressive lobbying to mitigate the influence of the tobacco industry. As time went on, major organizations including the American Medical Association would draw a more definitive line against smoking and tobacco use, with many of these groups advancing the cause to the legislative fronts.6
These efforts, combined with continued education of the public, led to several landmark changes that contributed, in a significant way, to declines in smoking and tobacco use. Including efforts that led to Federal Cigarette Labeling and Advertising Act in 1965, a broadcast ban on cigarette ads in 1971, introduction of cessation devices, such as nicotine gum and subsequent patches, in the 1980s and 1990s, bans on smoking in indoor and public places, and multiple lawsuits against the tobacco industry, including those from the Justice Department for what they considered a “coordinated campaign of fraud and deceit”.10
Now, 60 years on, the lessons learned echo in ongoing public health efforts.
In the latter half of the 20th century, as the nation was gripped with an HIV/AIDS epidemic, public health could lean on lessons learned in messaging and public education surrounding behavioral changes to try and manage this public health crisis. The rising issue of substance abuse has been confronted through a similar combination of education, policy changes, and community involvement.
During the COVID-19 pandemic, public health, once again, found itself relying on the lessons learned from the fight against smoking and tobacco use to inform their strategies, such as leveraging policy changes and information dissemination to encourage vaccination efforts.
“That’s just a measure of how our citizens working through public health organizations who advocate and speak to lawmakers can make a difference. Since that time, the same organizations have continued to advocate in multiple spheres of public health,” Rizzo added. “But these messages are really important because these messages have to be based in science and trust.”
Still, despite the success of public health efforts in curbing smoking and ushering in marked declines for both smoking and its related health conditions, a similar but nuanced issue has risen to the forefront of public health concerns and threatens to unravel some of this progress.
Vaping
As the community was commemorating the 50th anniversary of this report in 2014, unbeknownst to many, a new epidemic was preparing to emerge. The epidemic would take the form of electronic cigarette use, especially among young people in the US.
In 2019, there were about 2.9 million children who began using e-cigarettes, a number that surpassed previous years, and 69% of youth reported flavored e-cigarette use, with alarmingly high rates among high school and middle school students (72% and 60%, respectively). From 2011 - 2019, a dramatic uptick in current e-cigarette smoking was observed among middle schoolers and high schoolers, with increases of 1650% and 1733%, respectively.11
Rose Marie Robertson, MD
Credit: American Heart Association

“I think also the ability of people to use tobacco products—the newer tobacco product—in an invisible way. That was really, I suppose, one of the most surprising things,” said Rose Marie Robertson, MD, deputy chief science and medical officer of the AHA as well as the co-director of AHA’s Tobacco Center of Regulatory Science, when reflecting on the rise of vaping in the 21st century.
These statistics become even more alarming when considering the risks e-cigarettes pose for lung cancer and asthma. One ingredient found in these products is acrolein, an herbicide which can result in COPD or acute lung injury.12
Other harmful flavorings, nicotine, ultrafine particles, and heavy metals are also found in e-cigarettes, according to findings from a 2016 iteration of the Surgeon General report. This report highlighted the dangers of these ingredients, and consequently the FDA has not identified any e-cigarette as safe or effective for smoking cessation.12
This ascent of this new plague to the forefront of public health does share commonalities with the ascent of combustible forms of tobacco, including the flaunting of loopholes in marketing regulations and specific targeting of youth and minority communities. As a result, many involved in advocacy positions note the importance of regulatory and legislative reform in shifting the tide of this ongoing battle.
“With each of these reports, certainly it was true back 10 years ago and continues to be true, we see that there are surprises in them,” Robertson added. “And that the public can know a lot, but perhaps not know some critical item that is personally relevant to them.”
As the ascent shares similarities with that of the cigarette smoking that preceded it, many are hopeful the actions, both those put forth in the last decade and those ongoing, will pay dividends in a similar fashion as those which have proven so effective in the last 60 years.
“I think we ought to take lessons from the 1960s to get ahead of this and the idea is to develop a national campaign, where the current Surgeon General comes out and speaks in the same way about the ‘deleterious effects’ of vaping, particularly among young people,” Alcendor said.
References:
- National Institutes of Health. The 1964 report on Smoking and health | reports of the surgeon general - profiles in science. U.S. National Library of Medicine. Accessed January 31, 2024. https://profiles.nlm.nih.gov/spotlight/nn/feature/smoking.
- Centers for Disease Control and Prevention. Achievements in public health, 1900-1999: Tobacco use -- United States, 1900-1999. Centers for Disease Control and Prevention. November 5, 1999. Accessed January 31, 2024. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm4843a2.htm.
- Cornelius ME, Loretan CG, Jamal A, et al. Tobacco Product Use Among Adults — United States, 2021. MMWR Morb Mortal Wkly Rep 2023;72:475–483.
- Holford TR, Meza R, Warner KE, et al. Tobacco control and the reduction in smoking-related premature deaths in the United States, 1964-2012. JAMA. 2014;311(2):164-171. doi:10.1001/jama.2013.285112
- Centers for Disease Control and Prevention. Current cigarette smoking among adults in the United States. Centers for Disease Control and Prevention. May 4, 2023. Accessed January 31, 2024. https://www.cdc.gov/tobacco/data_statistics/fact_sheets/adult_data/cig_smoking/index.htm.
- National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Atlanta (GA): Centers for Disease Control and Prevention (US); 2014.
- Harvard Health. Surgeon general’s 1964 report: Making smoking history. Harvard Health Blog. January 10, 2014. Accessed January 31, 2024. https://www.health.harvard.edu/blog/surgeon-generals-1964-report-making-smoking-history-201401106970.
- Martin SS, Aday AW, Almarzooq ZI, et al. 2024 Heart Disease and Stroke Statistics: A Report of US and Global Data From the American Heart Association. Circulation. Published online January 24, 2024. doi:10.1161/CIR.0000000000001209
- Lloyd-Jones DM, Allen NB, Anderson CAM, et al. Life's Essential 8: Updating and Enhancing the American Heart Association's Construct of Cardiovascular Health: A Presidential Advisory From the American Heart Association. Circulation. 2022;146(5):e18-e43. doi:10.1161/CIR.0000000000001078
- American Lung Association. Tobacco control milestones: State of tobacco control. State of Tobacco Control | American Lung Association. Accessed January 31, 2024. https://www.lung.org/research/sotc/tobacco-timeline.
- American Lung Association. Tobacco trends brief. Tobacco Trends Brief | American Lung Association. Accessed January 31, 2024. https://www.lung.org/research/trends-in-lung-disease/tobacco-trends-brief/overall-tobacco-trends.
- American Lung Association. Health risks of e-cigarettes and vaping. Health Risks of E-Cigarettes and Vaping | American Lung Association. Accessed January 31, 2024. https://www.lung.org/quit-smoking/e-cigarettes-vaping/impact-of-e-cigarettes-on-lung.





