Article
A Drop of Ophthalmic a Day Could Keep Ptosis Surgery at Bay
Author(s):
A daily drop of oxymetazoline ophthalmic could avert surgery for acquired ptosis, according to new findings.
A daily drop of oxymetazoline ophthalmic solution demonstrated sufficient improvement in the visual impairment and cosmetic appearance of acquired ptosis for some patients to avoid corrective surgery, in a recently published analysis of data from two phase 3 trials which were pivotal for US Food and Drug Association (FDA) approval of the agent (Upneeq) in July.
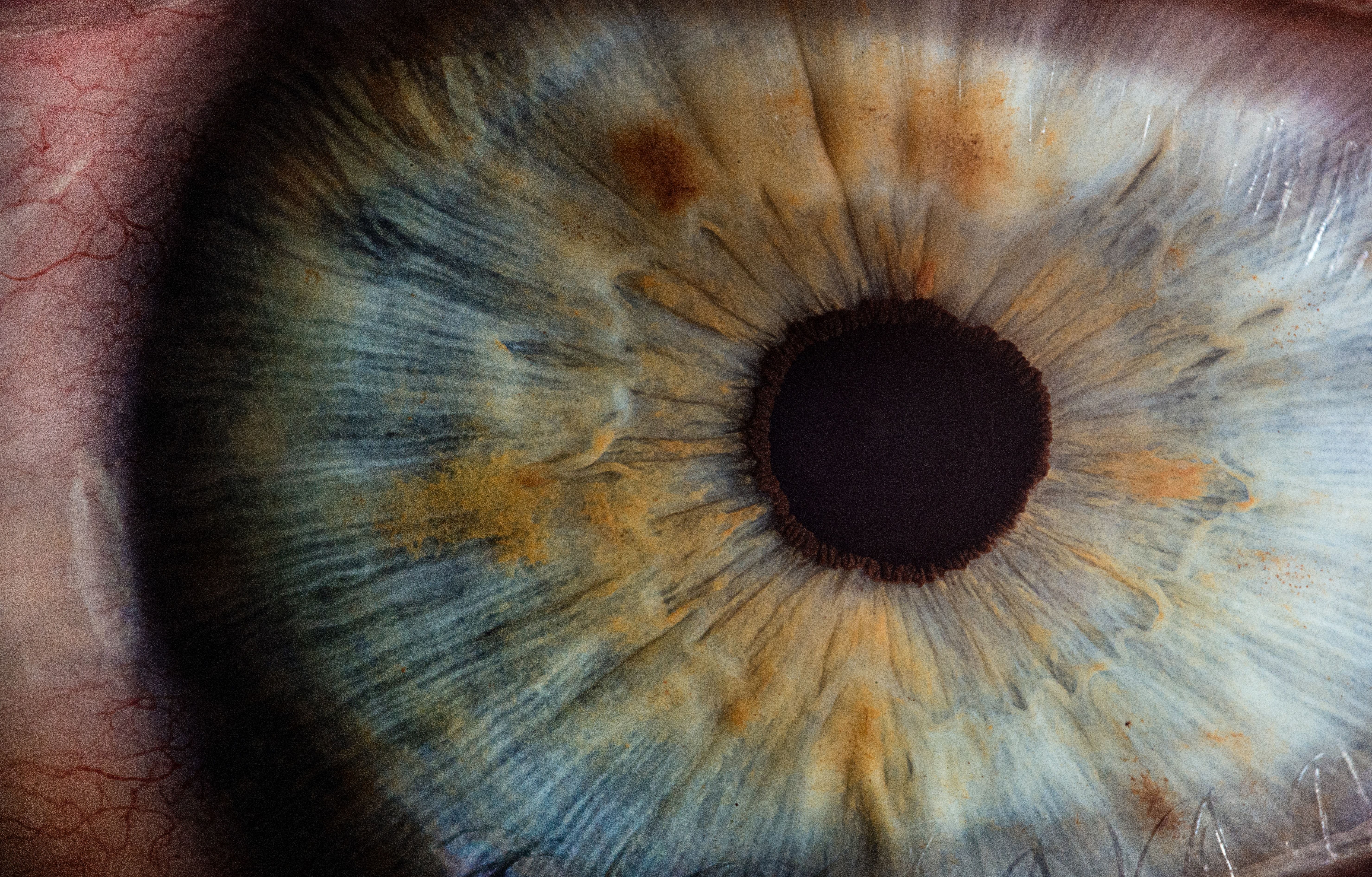
Charles Slonim, MD, Department of Ophthalmology, University of South Florida Morsani College of Medicine, and colleagues had reasoned that the target of standard surgery for acquired form of ptosis, the superior tarsel (Müller) upper eye-lid retractor muscle, can also be affected pharmacologically
“Because it expresses adrenergic receptors, Müller muscle is also a target for pharmacologic intervention,” Slonim and colleagues explained. “A limited number of studies have described the use of adrenergic drugs (phenylephrine, apraclonidine) for ptosis treatment.”
Oxymetazoline is an alpha adrenergic which has been available for several decades in a lower concentration spray to treat nasal congestion. The approval of a 0.1% ophthalmic solution for ptosis is described as an appealing repurposing of an old drug, in accompanying commentary by Elizabeth Bradley, MD, MHS, May Clinic Department of Ophthalmology, Mayo Foundation, and colleagues.
“An old drug comes with a known adverse effect profile and an established manufacturing base,” Bradley and colleagues observed. “However, proving that an old drug can safely and effectively take on a new role may not be easy.”
The 2 double-blind, placebo-controlled multicenter phase 3 clinical trials randomized a total of 203 participants to receive oxymetazoline 0.1% ophthalmic solution and 101 to receive the vehicle without active ingredient. Participants had demonstrated impaired superior visual field by inability to detect at least 8 of 17 points in the top 2 rows on the Leicester Peripheral Field Test (LPFT); and deficient upper eyelid height, measured as marginal reflex distance 1 (MRD-1).
The oxymetazoline or inactive vehicle was self-administered once daily in the morning for up to 42 days. Assessments, including the LPFT and MRD-1 were made at baseline before treatment, at 6 hours after administration on day 1, and at 2 hours after administration on day 14. The six- and two-hour time intervals were used to assess duration and onset of effect, respectively.
Slonim and colleagues reported that the oxymetazoline was associated with a statistically significant increase in the mean number of points seen on the LPFT, and significantly more than with the vehicle solution. The active agent was also associated with a significant increase in MRD-1 relative to baseline. Treatment emergent adverse event occurred in 31.0% of the oxymetazoline group and 35.6% of those receiving the inactive vehicle.
Slonim and colleagues conclude that the data with oxymetazoline opthalmic solution demonstrate its "potential promise for the treatment of acquired ptosis, although further study is needed to elucidate the clinical relevance of these findings beyond 6 weeks."
Bradley and colleagues observe that the trials were also too brief to allow for full assessment of adverse effects, "including known alpha adrenergic agonist adverse effects of follicular conjunctivitis and dry eye."
The commentators welcome the potential for a pharmacological option to surgery, however. "Surgery is not without possible unwanted effects, including dry eye, lagophthalmos, and overcorrection or undercorrection," they noted.
The pooled analysis of 2 randomized clinical trials, "Association of Oxymetazoline Hydrochloride, 0.1%, Solution Administration with Visual Field in Acquired Ptosis" were published online in JAMA Ophthalmology.