Article
AHA Calls Attention to Growing Impact of NAFLD on Cardiovascular Disease Risk
Author(s):
The latest scientific statement from the American Heart Association is aimed at improving the awareness of NAFLD and its associated cardiovascular risk among clinicians as well as optimizing diagnosis and early treatment strategies for patients with NAFLD.
P. Barton Duell, MD

The American Heart Association is hoping to draw attention to an overlooked issue impacting the cardiovascular health of millions worldwide with their latest scientific statement: nonalcoholic fatty liver disease (NAFLD).
With previous data suggesting NAFLD could be affecting 25% of adults worldwide, the AHA’s scientific statement is aimed at increasing awareness around NAFLD as well as facilitate improved diagnosis and early treatment effort to help reduce the impact NAFLD can have on cardiovascular disease risk on a societal level.
“Nonalcoholic fatty liver disease is a common condition that is often hidden or missed in routine medical care. It is important to know about the condition and treat it early because it is a risk factor for chronic liver damage and cardiovascular disease,” said P. Barton Duell, MD, FAHA, chair of the statement writing committee and professor of medicine in the Knight Cardiovascular Institute and Division of Endocrinology, Diabetes and Clinical Nutrition at Oregon Health & Science University, in a statement from the AHA.
Published on April 14 and citing more than 160 reference documents, the statement composed by Duell and colleagues was prepared by the volunteer writing group on behalf of the American Heart Association’s Council on Atherosclerosis, Thrombosis and Vascular Biology, the Council on Hypertension, the Council on the Kidney in Cardiovascular Disease, the Council on Lifestyle and Cardiometabolic Health, and the Council on Peripheral Vascular Disease. At 18 pages in length, the document dedicates 10 subsections to outlining terminology, risk factors for NAFLD, Pathogenesis of NAFLD, predisposing genetic risk factors, NAFLD and atherosclerotic cardiovascular disease risk, NAFLD in patients undergoing PCI and CABG, hypobetalipoproteinemia and NAFLD, Safety of statins in NAFLD, strategies for screening of NAFLD and NASH, and potential interventions for NAFLD.
A large portion of the statement was dedicated to interventions for NAFLD, both from a pharmacological perspective and also addressing modifiable risk factors. In addition to dietary and lifestyle modification, authors underlined the importance of using proven agents, such as GLP-1 RAs, metformin, and lipid-lowering therapies, among patients with NAFLD or NASH. In addition to providing information on established therapies, the writing committee also offered insight into the potential for experimental agents from contemporary data.
“Part of the good news about managing NAFLD is that healthy eating, regular exercise and weight loss or avoiding weight gain are all valuable interventions to improve health in most of us, regardless of whether we have NAFLD,” said Duell.
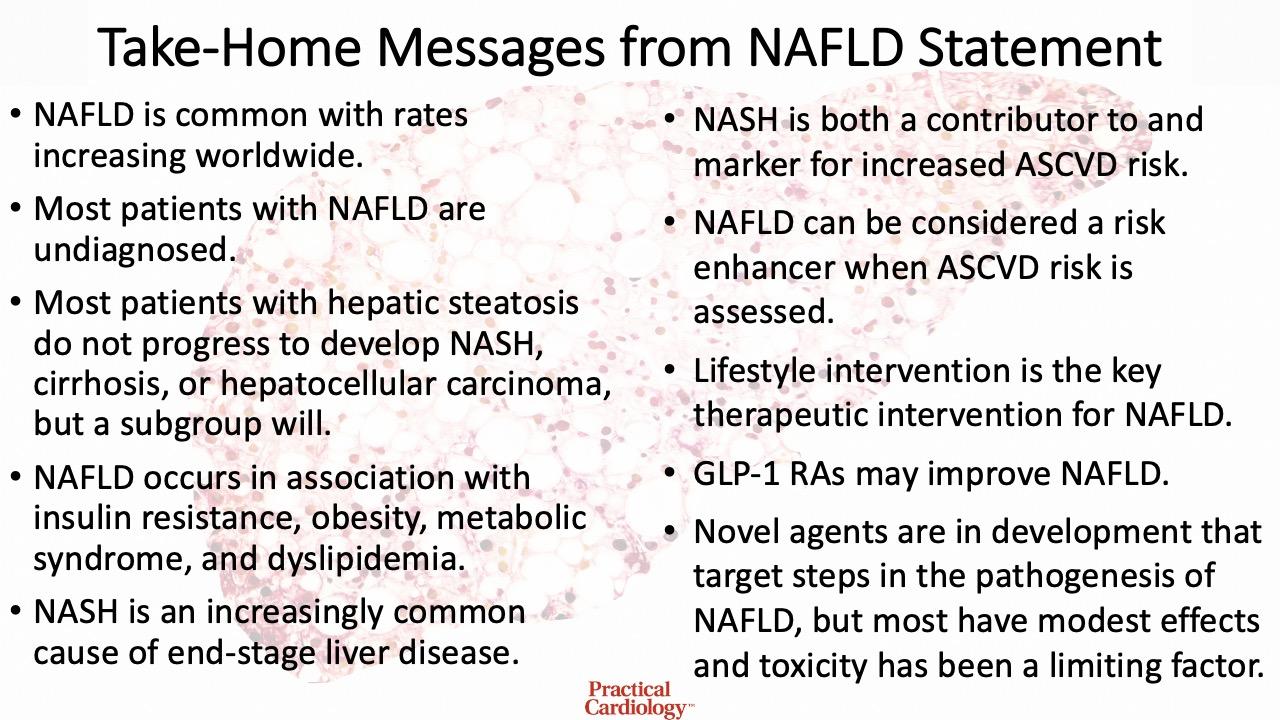
In their conclusion, authors provided clinicians with their top take-home messages from the statement, which are summarized in the graphic below.
Summary of the top take-home messages from the AHA's scientific statement on NAFLD's role in cardiovascular disease risk.
This statement, “Nonalcoholic Fatty Liver Disease and Cardiovascular Risk: A Scientific Statement From the American Heart Association,” was published in Arteriosclerosis, Thrombosis, and Vascular Biology.





