Article
Alcoholic Hepatitis: Filtering Device Helped Younger, Less Ill Patients
Author(s):
A human-cell-based liver support system meant to keep patients alive despite acute liver failure did not help overall survival in a trial, but showed promise for a subset of patients. Those patients were younger and not as sick-though all subjects enrolled had alcoholic hepatitis.
A human cell-based liver support system meant to keep patients alive despite acute liver failure did not help overall survival in a trial, but showed promise for a subset of patients. Those patients were younger and not as sick—though all subjects enrolled had alcoholic hepatitis.
In data to be presented in a late-breaking abstract at the Liver Meeting (AASLD) in San Francisco, CA, Julie Thompson, MD, of the University of Minnesota Medical Center in Minneapolis, MN and colleagues reported on a multi-center study of the device system, known as ELAD (Vital Therapies, San Diego, CA.)
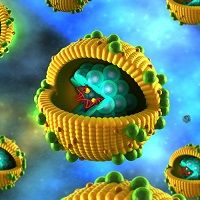
Similar in concept to kidney dialysis, the device filters patients’ blood outside the body, much as the liver does inside. But it uses a human cell line derived from the liver.
These proprietary cells (VTL C3A cells) are contained in four hollow fiber cartridges.
During treatment with the ELAD System, blood is drawn from the patient via a central venous line and then passes into an ancillary delivery system. There plasma ultrafiltrate is isolated by an ultrafiltrate generator. The patient’s plasma ultrafiltrate then passes into the four cartridges where it contacts the VTL C3A cells after passing through fibers which allow appropriate two-way transfer of toxins, metabolites and nutrients, mimicking liver function. The fibers, made of a semi-permeable membrane, permit passage of macromolecules and other substances from the VTL C3A cells to the patient’s plasma ultrafiltrate. At the same time, these fibers permit the passage of toxins such as bilirubin, and nutrients such as glucose, and oxygen from the plasma ultrafiltrate, to the VTL C3A cells.
Patients also get heparin during the procedure. Treated blood is returned to the patient via a central line. Administering the therapy takes between three and ten days of continuous treatment.
The study involved 203 patients of whom 96 got treatment with the ELAD device and 107 got standard care. There were 40 centers involved.
Though there was no significant difference in overall survival, “subgroup analysis strong trends toward improved survival in groups in which MELD scores or age were lower that the baseline for the group.
With patients whose MELD score was less than 28, overall survival with ELAD was 71% vs. 57% for those who got standard care. Younger patients also did better with a 67% survival on ELAD vs 55% on standard care.
For the patients who had both lower MELD scores and were younger, survival was 100% on ELAD vs. 73% with standard care.





