Article
Anifrolumab Shows Efficiency in Systemic Lupus
Author(s):
In patients with moderate to severe systemic lupus erythematosus (SLE), anifrolumab (AstraZeneca) was superior to placebo for improving overall disease activity, skin disease and oral corticosteroid tapering, say researchers writing in the New England Journal of Medicine.
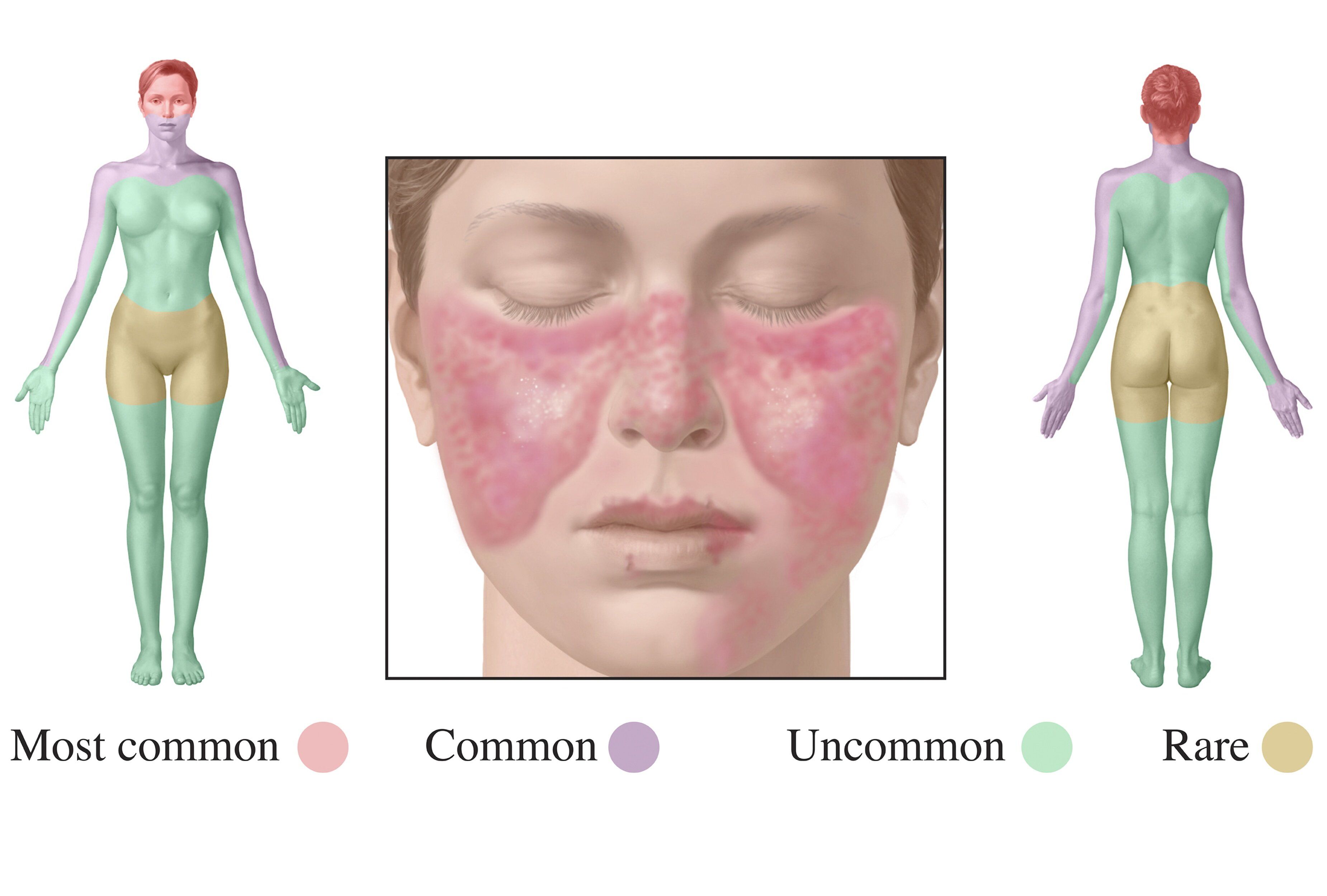
(©MedicalIllustrations.com, 01AQM661)
In patients with moderate to severe systemic lupus erythematosus (SLE), anifrolumab (AstraZeneca) was superior to placebo for improving overall disease activity, skin disease and oral corticosteroid tapering, say researchers writing in the New England Journal of Medicine.
Despite the approval of belimumab for the treatment of SLE, the condition is associated with clinical burden for the patient and organ damage. The development of therapies for SLE has been constrained by clinical and biologic heterogeneity, including diversity of peripheral-blood gene expression signatures, representing challenges in trial design and end-point selection that may have contributed to SLE study failures.
Anifrolumab, a human monoclonal antibody to the type I interferon receptor subunit 1, showed efficacy in a phase two study of patients with active SLE. While the first phase three trial, TULIP-1, did not meet its primary endpoint, multiple secondary endpoints, including BILAG–based Composite Lupus Assessment (BICLA), suggested clinical benefit.
“We report the findings of TULIP-2, a second phase three trial of anifrolumab in active SLE using the BICLA secondary end point from the first phase three trial as its primary end point,” wrote the authors, led by Eric Morand, M.D., of Monash University in Australia.
TULIP-2 included 362 lupus patients who were randomly assigned to receive intravenous anifrolumab 300 mg (n=180) or placebo (n=182) every four weeks for 48 weeks. The primary end point was BICLA response at week 52. Secondary end points included a BICLA response in patients with a high interferon gene signature at baseline; reductions in the glucocorticoid dose, in the severity of skin disease, and in swollen and tender joint counts; and the annualized flare rate.
RELATED: "Lupus Trial for Anifrolumab Gets a Second Look"
Anifrolumab was superior to placebo for BICLA response (47.8 percent vs 31.5 percent, respectively, P=0.001). Among patients with a high interferon gene signature, the response rate was 48.0 percent in the anifrolumab group and 30.7 percent in the placebo group; among patients with a low interferon gene signature, the response rate was 46.7 percent and 35.5 percent, respectively. For secondary end points, the glucocorticoid dose and the severity of skin disease, but not swollen and tender joint counts, and the annualized flare rate, showed a significant benefit with anifrolumab. Herpes zoster and bronchitis occurred in 7.2 percent and 12.2 percent of the patients, respectively, who received anifrolumab. 0ne death from pneumonia occurred in the anifrolumab group.
“The TULIP-2 trial showed that anifrolumab (at a dose of 300 mg administered intravenously every four weeks) in patients with active SLE was superior to placebo in the achievement of composite end points of disease-activity response, as well as reduction in the glucocorticoid dose and reduction in the severity of skin disease, over a period of 52 weeks,” the authors wrote.
“Suppression of the interferon gene signature was observed in patients receiving anifrolumab who had a high interferon gene signature at baseline, although any putative association between this effect and clinical efficacy has not been investigated,” wrote the authors. Due to the small number of patients who had low interferon gene signature at baseline, “the effect of anifrolumab in such patients requires further analysis.”
REFERENCE
Eric F. Morand, Richard Furie, Yoshiya Tanaka, et al. “Trial of Anifrolumab in Active Systemic Lupus Erythematosus.”NEJM. January 16, 2020. doi: 10.1056/NEJMoa1912190




