Article
Anticoagulation by the Book: A 3-Case Challenge
If, when, and for how long anticoagulation should be administered in these 3 patients is the challenge in each case. Do you know your guidelines?
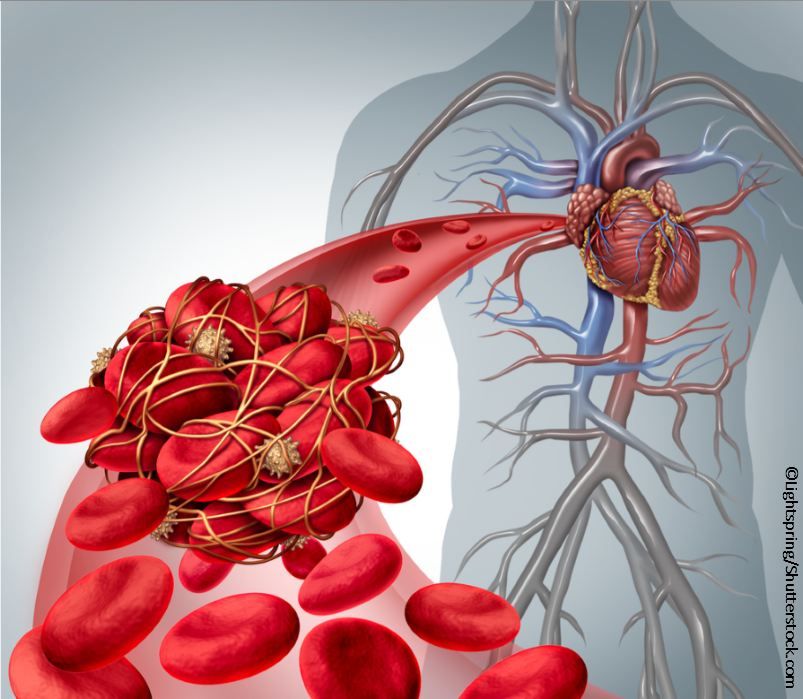
©Lightspring/Shutterstock.com
Case 1: A 75-year-old woman with a history of obesity, obstructive sleep apnea (OSA), and hypertension (HTN) has an episode of atrial fibrillation (AF) during hospitalization for a bacterial pneumonia. The episode lasts for 3 days and then she spontaneously reverts to normal sinus rhythm.
Does she need anticoagulation? If so, for how long?
Please click below for answers and Case 2.
Answers:
Short-term anticoagulation: Although the risk of thrombus formation increases as early as a few minutes following onset of the arrhythmia, studies suggest that AF of <48h duration does not need to be anticoagulated. For episodes >48h, the CHA2DS2-Vasc scoring system should be used to determine the underlying risk of thromboembolism and need for anticoagulation. Just as with paroxysmal AF, anyone with a CHA2DS2-Vasc score ≥2 needs oral anticoagulation. This patient’s score is 3 (age, female, HTN) and the episode of AF was >48h. She should receive oral anticoagulation therapy.
Long-term anticoagulation: Until recently, AF treatment guidelines allowed for an episode of “lone” AF, meaning short duration AF that could represent an isolated occurrence of AF. Newer guidelines, however, suggest that even a single episode of AF warrants aggressive long-term anticoagulation (based on CHA2DS2-Vasc ≥2 risk stratification) since it suggests the ability of the atria to sustain the arrhythmia. In this case, the episode of AF may have been triggered by conditions related to the pneumonia but her underlying risk factors (HTN, obesity, OSA, age) suggest that she has multiple risk factors for atrial fibrillation.
****************************************Case 2: A 52-year-old man presents with a first occurrence of symptomatic AF of unknown duration and agrees to proceed with cardioversion.
What are recommendations for anticoagulation for this patient prior to the procedure if it is:
A. Performed immediately
B. Performed at a later time
Please click below for answers and Case 3
Answers:
Immediate cardioversion. If immediate cardioversion is desired (because AF begets more AF) then a TEE (transesophageal echocardiogram) should be performed prior to cardioversion to rule out left atrial appendage thrombus.
Delayed cardioversion. If cardioversion can be delayed for 1 month, then 4 therapeutic INRs or anticoagulation with one of the novel oral anticoagulants for 4 weeks should be undertaken.
****************************************Case 3: An 87-year-old woman with HTN, CHF, prior stroke, and persistent AF [on warfarin] presents with her third GI bleed in 6 months. This time, she required 3 units packed red blood cells.
How would you proceed with anticoagulation therapy for this patient at this time?
Please click below for answer.
Answer:
Given her recurrent GI bleeds and ongoing risk factors for thromboembolism in the setting of persistent AF, this patient meets indications for oral anticoagulation. However, with the recurrent bleeding, this is relatively contraindicated. Therefore, she would be a good candidate for a left atrial appendage occlusion device (ie, Watchman device), which has been approved for patients with non-valvular AF as an alternative to warfarin therapy for reducing the risk of stroke.
Sources:
January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. JACC. 2014;64: 2246-2280.
Wyse GD, Van Gelder IC, Ellinor PT, et al. Lone atrial fibrillation: does it exist? [white paper]. JACC. 2014;63:1715-1723





