Article
Are radiographic axSpA and ankylosing spondylitis one in the same?
The established criteria for radiographic axial spondyloarthritis and axial spondyloarthritis that is classified as ankylosing spondylitis-is essentially the same, report physicians who recommend the interchangeable use of the terms "ankylosing spondylitis" and "radiographic axial spondyloarthritis."
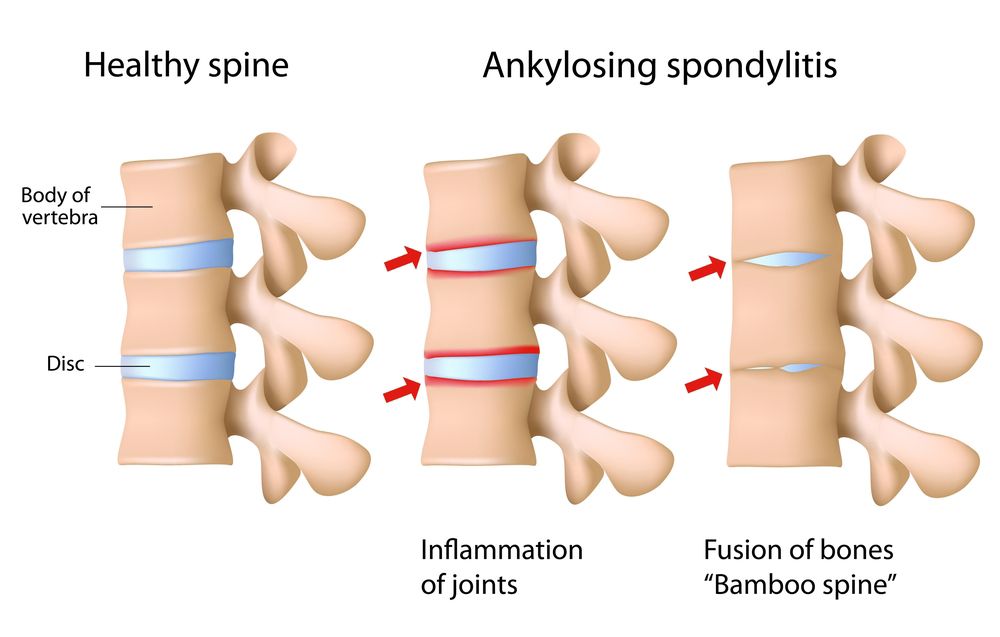
(©AlilaMedicalMediaShutterstock.com)
The established criteria for radiographic axial spondyloarthritis and axial spondyloarthritis that is classified as ankylosing spondylitis-is essentially the same, report physicians who recommend the interchangeable use of the terms "ankylosing spondylitis" and "radiographic axial spondyloarthritis."
The recommendation is based on the results of an analysis in which researchers examined the results of eight studies including 3,882 patients who fulfilled the modified New York (mNY) criteria for ankylosing spondylitis (AS) and 3,434 patients who met the criteria for the Assessment of SpondyloArthritis international Society (ASAS) criteria as radiographic axial spondyloarthritis (r-axSpA).
They found that 93 percent of those who met the mNY criteria also met the ASAS criteria for radiographic axial spondyloarthritis and 96 percent of those patients met the mNY criteria.
The study, which was led by Anne Boel of Leiden, Netherlands, appears in the July 30 online issue of the Annals of the Rheumatic Diseases.
“Acknowledging that r-axSpA and AS are interchangeable increases comparability between studies, since both terms describe the same patients (ie, patients with axSpA with radiographic sacroiliitis),” the authors wrote.
While both the modified New York criteria and ASAS criteria use the same radiographic evidence, they differ in the clinical features required to make the diagnosis. One of the major differences is that patients who are diagnosed at 45 years or later, do not fulfill the international society criteria, while there is no age limit for the modified New York criteria.
The authors sought to determine if the two sets of criteria were in fact classifying the same patients.
“Classification criteria are standardized definitions that are primarily intended to create well-defined, relatively homogeneous cohorts of patients for clinical research; they are not intended to capture every single patient but rather to capture the majority of patients who share key features of the condition,” the authors wrote.
Take-home points for clinicians and final thoughts
While diagnostic criteria are designed to categorize patients for research and treatment purposes, even minor disagreements can cause confusion. In this study, the age at onset of back pain criteria appears to be the factor separating two similar diagnostic groups who in fact represent the same population.
This study highlights the perils of multiple classification criteria being developed for similar signs and symptoms without collaboration and often in different countries. Comparing the criteria as the authors have done, allows researchers to build on each other’s work even when not in close proximity to each other.
The authors state, “This also ensures that results from older research on AS cohorts can be directly compared with more recently published articles on r-axSpA cohorts.”
Collaboration is at the heart of medical advancement. Rheumatologic disorders including spondyloarthritis are complex by nature requiring a great deal of collaboration with research building on prior investigations to produce advancements in diagnosis and treatment.
The author’s efforts should bring together a wider body of research and pave the way for groundbreaking work in essence dramatically increasing the sample size for axial spondyloarthritis patients by combining the diagnoses of ankylosing spondylitis and radiographic axial spondyloarthritis.
REFERENCE
Boel A, Molto A, van der Heijde D, et al. “Do patients with axial spondyloarthritis with radiographic sacroiliitis fulfil both the modified New York criteria and the ASAS axial spondyloarthritis criteria? Results from eight cohorts.” Annals of the Rheumatic Diseases. Published Online First: 30 July 2019. doi: 10.1136/annrheumdis-2019-215707




