Article
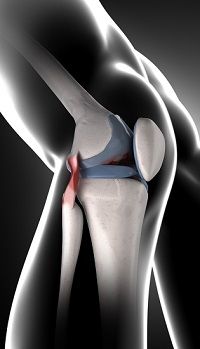
Arthritis Could Be Delayed With Molecule Retention
Author(s):
A study of ACL-damaged rats shows molecular development of arthritis.
Forms of arthritis could be prevented by the retention of a molecule that nourishes cartilage.
Adenosine, a biochemical pivotal in human cellular function, is capable of retaining healthy forms of these cells, called chondrocytes, according to a recent study.
Adenosine is derived from triphosphate (ATP), a molecule that stores energy needed by the body’s cells until it is used, according to the study. While it has been known that inflammation and aging diminishes ATP production in chondrocytes, there had not been a link from diminished adenosine levels to osteoarthritis until this study.
The study, conducted by New York University (NYU) Langone Medical Center researchers, found that maintaining high levels of adenosine in rats inflicted with anterior cruciate ligament (ACL) damage prevented them from developing the common form of “wear and tear” arthritis.
Adenosine replacement therapy could potentially delay osteoarthritis in humans and lessen needs for joint replacements, researchers said.
“We found that if adenosine levels decrease, or if the capacity to respond to adenosine diminishes, cartilage starts to degenerate,” senior investigator Bruce Cronstein, MD, the Dr. Paul R. Esserman Professor of Medicine at NYU Langone, said.
Cronstein and his team’s research suggests that reductions in the amount of cartilage-producing cells — and the greater risk for osteoarthritis — may be driven by both lower adenosine levels and lower protein levels on the surface of chondrocytes that are designed to receive and pass on adenosine signals.
Adenosine sustains cells by fitting into the surface of A2A adenosine receptor proteins, like a lock into a key, according to the study. Mice studied in the research did not walk as easily as mice with the receptor, and examination of the mice without the receptor showed they had osteoarthritis.
Levels of adenosine A2A receptors went up on rat chondrocytes when osteoarthritis was present, according to the study. This indicated a “failed attempt” to compensate for adenosine loss from the metabolic changes underlying inflammation.
In tissue sample tests from osteoarthritic patients who had joint replacements, researchers saw similarly increased levels of adenosine A2A receptors on chondrocytes.
After treating mouse chondrocytes with a molecule called IL-1beta — which has been shown to contribute to the development of osteoarthritis — ATP production in the chondrocytes was lessened by 39%. There was also an 80% less expression from ATP-exporting molecule ANKH.
Researchers finally found that the lack of enzyme that turns ATP into adenosine diminished adenosine levels, leading to mice osteoarthritis. The lack of enzyme is known to lead to the disease in humans.
The researchers found that excess adenosine prevented the development of osteoarthritis in animals, after researchers administered lipid bubbles into the site of rats’ ACL injuries.
Related future therapies could entirely prevent or delay the need for joint replacements, which are administered to millions annually.
“Because joints may have to be replaced again and again, if we can put off the need for joint replacement until late in life, odds are that patients will only have to have this done once,” Cronstein said.
The study was published earlier this month in the journal Nature Communications.
A press release regarding the study was made available.
Related Coverage:
Rewired Stem Cells Could Provide Their Own Arthritic Drug, Research Finds
Pfizer Seeks to Expand Tofacitinib Approval to Include Psoriatic Arthritis




