Article
ASH Data Points to Correlation Between Biomarkers and Sickle Cell Outcomes
Author(s):
In a study presented at the annual ASH meeting, investigators link biomarkers of cardiopulmonary, renal, and liver dysfunction with specific outcomes for adult sickle cell disease patients.
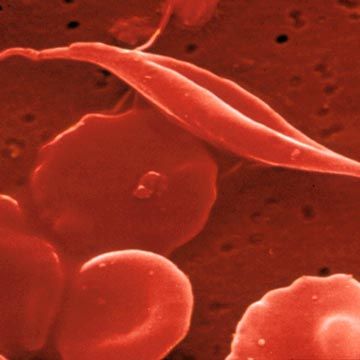
Using various sickle cell disease etiological conditions, investigators have identified several biomarkers associated with different cardiopulmonary, renal, and liver dysfunction outcomes.
A team of investigators, led by Xu Zhang, PhD, Department of Medicine, University of Illinois at Chicago, examined the correlation of biomarkers that reflect major aspects of the sickle cell disease patho-physiology—hemolysis, anemia, hypoxia, inflammation, and iron overload—with cardiopulmonary, renal, and live dysfunction in adult patients.
The study, which was presented at the American Society of Hematology (ASH) 2019 annual meeting, provides observational evidence for the etiologies of sickle cell organ damage by assessing the relative strength of outcomes linked to the biomarkers.
A total of 442 adult patients with sickle cell disease were included in the cohort study. The median age of the patients in the study was 31 years old and 77% of the patients had severe β hemoglobin mutation genotypes (HbSS, HbSβ0-thalassemia, HbSOarab).
For those suffering from sickle cell disease, chronic anemia, hypoxia, and nitric oxide scavenging related to intravascular hemolysis is linked to diastolic dysfunction and pulmonary hypertensions. Free hemoglobin, along with heme released during hemolysis can cause oxidative stress and exacerbate vascular inflammation.
Iron overload from frequent blood transfusions also provoke oxygen species, leading to cellular damage.
Primary cardiopulmonary outcomes were left heart enlargement—left atrial and ventricular diameter—and elevated systolic pulmonary artery pressure measured by tricuspid regurgitation peak velocity (TRV). The primary renal outcome was elevated urine albumin to creatinine ratio (ACR) and estimated glomerular filtration rate (eGFR) <60 ml/min/1.73m2.
The primary hepatic outcomes were hepatocyte integrity estimated as the first principal component of alanine transaminase (ALT) and aspartate aminotransferase (AST), cholestasis estimated as the first principal component of alkaline phosphatase and direct bilirubin, and functioning liver mass measured by serum albumin.
The investigators examined the clinical associations between biomarkers and primary outcomes using single marker regression analysis with covariates of age, gender, and severity of β hemoglobin genotype.
Significant biomarkers representative of the major etiological conditions was analyzed using multi-marker regression and model selection.
“Left atrial diameter showed significant associations with biomarkers of hemolysis (LDH, percent reticulocytes, AST, total bilirubin), anemia (HCT, HGB), hypoxia (HCT, HGB, O2 saturation), and inflammation (WBC),” the authors wrote. “Left ventricular diameter had a profile of biomarker associations similar to left atrial diameter. RV showed significant associations with biomarkers of hemolysis (LDH, percent reticulocytes, AST), anemia (HCT, HGB), hypoxia (HCT, HGB, O2 saturation), inflammation (WBC), and iron overload (ferritin).”
In the multi-marker analysis, the investigators found that anemia and hypoxia (low HCT, low O­­2 saturation) was associated with greater left atrial diameter and high TRV.
Urine ACR was also substantially associated with biomarkers of hemolysis (LDH, AST, percent reticulocytes), anemia (HCT, HGB), hypoxia (HCT, HGB, O2­ saturation), inflammation (WBC, serum albumin), and iron overload (ferritin).
Cholestasis had a profile of biomarker associations similar to decreased hepatocyte integrity.
Functioning liver mass was significantly linked to decreased hepatocyte integrity, while anemia (low HCT) and iron overload (high ferritin) was associated with cholestasis and low functioning liver mass.
“Our study indicated significant correlations of anemia and hypoxia with both left heart enlargement and elevated pulmonary arterial systolic pressure,” the authors wrote. “Our study also underscores a significant impact of iron overload on renal and liver damages.”




