Article
The Balancing Act of Opioid Prescribing Guidelines
Author(s):
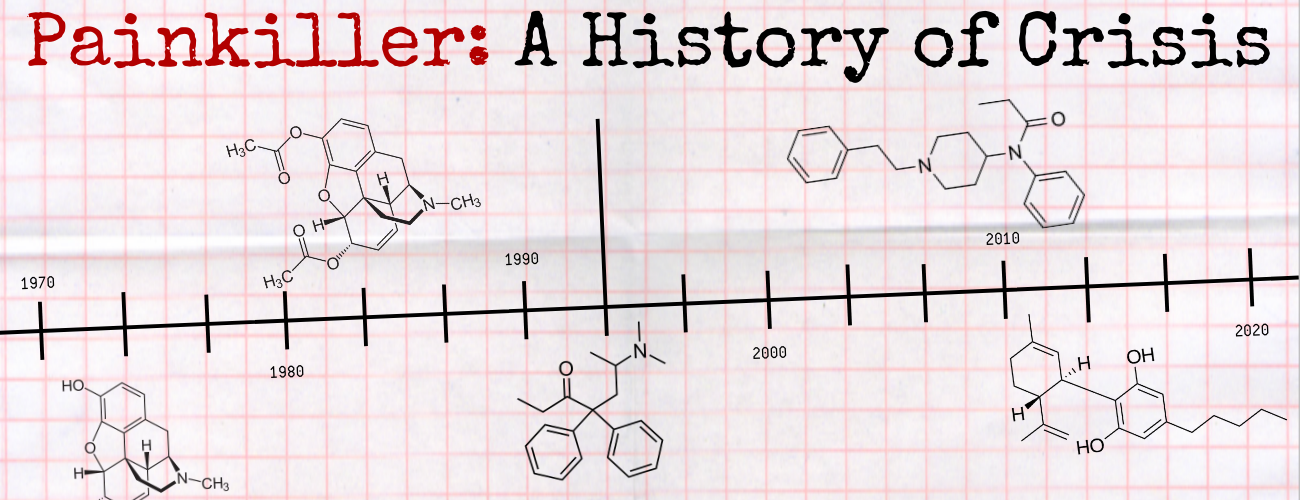
In part 4 of our series, guideline authors and researchers relay the particularities of guiding and regulating the spread of still-necessary painkiller prescriptions.
Last year, Russell Portenoy, MD, agreed to testify against Purdue Pharma, the maker of oxycontin, and other drug companies in state- and county-level lawsuits for their roles in the opioid epidemic.
This was an interesting development in the era of legal comeuppance for opioid developers: Portenoy was a longtime ally of Purdue, and was among the contracted physicians to play a large role in driving the growth of the use of addictive pain medication in the US. He was even a named defendant in litigation against other opioid developers, including Endo and Mallinckrodt.
Portenoy, a professor at the Albert Einstein College of Medicine, was one of the first physicians to support the use of opioids as a potential treatment for chronic pain, in medical journals published in the 1980s and 90s. Traditionally, physicians were trained to prescribe opioids for cancer treatment and end-of-life pain.
Portenoy was paid to promote opioids by making positive statements about them. He often did so without providing clinical background, analysis, and cautions that went hand-in-hand with what he was preaching. His promotion of the drugs encouraged opioids to be prescribed to patients who did not necessarily need them, by providers who did not know how to properly manage potential addiction, abuse, and overdose.
Prosecutors said they would drop lawsuits against Portenoy if he cooperated with their cases. He did, and in turn testified that drug makers did help create the opioid epidemic by failing to acknowledge the risks of abuse. In the lawsuit against the pharmaceutical companies, Portenoy is on record citing the aggressive promotion of the drugs for a wide array of ailments.
What’s more, he highlights the disservice he and his colleagues made in lapsing judgement on prescribing the drugs.
“If marketing is done that suggests to (patients) that pain relief is a possibility, they’re going to focus on that, they’re going to bring the information to their physician, and are going to ask for these drugs,” Portenoy testified. “They have to be hopeful that their physician had been adequately educated and has the ability to say no to a patient who, perhaps assertively, says ‘Treat me, I have terrible pain.’ That just increases the risk that patients are going to get access to opioids and suffer negative consequences.”
Clinical care is built on structures and principles driven by evidence-based research, patient needs, and expert opinion. In 2020, opioids are still needed and prescribed in pain management. That is not changing anytime soon.
The Reality of the Opioid Epidemic
While public health agencies and legislation has largely embraced the battle to combat the spread of drug addiction and abuse in the US, it is the familiar healthcare agencies that have tasked themselves with refining and enforcing a modernized prescribing strategy.The harrowing reality is that 80% of people using heroin started with a prescription to another opioid, according to the Addiction Center. The problem, then, is exacerbated by over-prescribing, along with the highly addictive nature of painkillers.
The US Centers for Disease Control and Prevention (CDC) identified prescription opioid addiction and overdose as the “first wave” of the epidemic—eventually feeding into the second wave of heroin abuse once treated patients sought a new high or unregulated access to drugs.
Though prescription overdose deaths have decreased annually, the CDC reports 130 Americans still die daily from the product. The country is onto the second and third wave of the epidemic—illicit and synthetic drugs—but its root problem still comes from the first wave of prescribing.
As with most other public health issues, regulatory response has been to establish clinical guidelines.
Baseline Rules
It should come as no surprise that federal agencies have led the charge into establishing opioid prescribing practices. As of today, guidelines include variations from the CDC; the US Department of Health and Human Services (HHS); and the US Food and Drug Administration (FDA). All medical boards also have their own guidance, but there is not much variability between them.
The CDC published its guideline, titled “CDC Guideline for Prescribing Opioids for Chronic Pain,” in 2016 to provide recommendations for primary care clinicians who prescribe opioids for chronic pain outside of active cancer treatment, palliative care, and end-of-life care. The agency established the guidance to address when to initiate or continue opioids for chronic pain; opioid selection, dosage, duration, follow-up, and discontinuation; and assessing risk and addressing harms of opioid use.
“This guideline is intended to improve communication between clinicians and patients about the risks and benefits of opioid therapy for chronic pain, improve the safety and effectiveness of pain treatment, and reduce the risks associated with long-term opioid therapy, including opioid use disorder, overdose, and death,” the agency wrote.
Open-Ended Care
But the guidelines drew ire from at least one physician-led organization, which charged that such recommendations were evolving into regulation—written by individuals with little to no real-life opioid prescribing expertise.Despite having a very prevalent role in US healthcare for 3 decades, research and clinical understanding of opioids is still developing. It only makes sense to have similarly adjusted guidance.
Laxmaiah Manchikanti, MD, board chairman and chief executive officer of the American Society of Interventional Pain Physicians (ASIPP), was the lead author of the organization’s 2017 opioid prescription guidance, “Responsible, Safe, and Effective Prescription of Opioids for Chronic Non-Cancer Pain: American Society of Interventional Pain Physicians Guidelines.”
Along with stressing the consistent use of comprehensive patient assessment prior to prescribing opioids, Manchikanti and colleagues stress the significance of variability in care for prescribing physicians—something lacking in the 2016 CDC chronic pain opioid prescription guidelines.
“All in all, we feel that the guidelines are pretty reasonable, and they can be followed without any major interruption in the delivery of care,” Manchikanti told HCPLive. “The guidelines offer various means with which to curb opioid abuse, but at the same time keeps access to patients who require them.”
Manchikanti explained that if guidelines such as those set by the CDC are not followed by medical boards—which essentially establish physician regulations—it can ultimately affect their licensure.
He and a team of physicians published their guidelines 1 year after the CDC’s, providing a more consistent philosophy among those interested in appropriately prescribing opioids. They are intended to provide a systematic and standardized approach to prescribing and pain management, with recognition that each provider and patient scenario is unique.
The ASIPP guidelines contain practices for prescribers, which start with a comprehensive assessment of the patient to decide whether the patient needs and is an appropriate candidate for opioids.
It is strongly recommended that prescribers begin with the assessment and documentation and then screen for opioid abuse to identify drug abusers. Patients with addiction potential are considered high-risk, and while the prescriber monitors their adherence during treatment, “it is crucial that these patients are followed more closely and monitored appropriately,” Manchikanti said.
If the prescriber identifies abnormalities in their usage patterns, they can be weaned off the medication or provided other medication-assisted treatments using buprenorphine. Patients can also be sent to addiction facilities or treated with non-opioid techniques.
Prescribers are also recommended to use prescription drug monitoring programs. The organization also strongly suggests that prescribers establish appropriate physical and psychological diagnoses.
During the screening and prescribing process, providers must assess the effectiveness of long-term opioid therapy, usually by starting with and monitoring low-dose, short-acting drugs. Long-acting or high-dose medication should only be given out in specific circumstances with severe intractable pain, per the guideline.
The initial screening process could be difficult, as some patients could exaggerate about their pain level and medical history. Although it is difficult to identify them outright, based on their previous behaviors, prescribers should be able to tell. Typically, the patients often have other abnormalities, like abnormal urine drug screening or a history of going to multiple doctors.
Patients also need to be educated on the effectiveness and adverse consequences of the opioids, while providers monitor for adherence, abuse, and noncompliance.
A Systemic Change for the Individual
Overdoses are still going to occur, and hurdles still persist for patients to receive timely addiction treatment. In fact, recent study findings showed less than one-third of adolescents to experience an opioid overdose ever did receive such care.
Study author Rachel Alinsky, MD, MPH, told HCPLive that providers often do not know if their patient is presenting with opioid use disorder, or how to help get them treatment when they do recognize it.
Alinsky, from the general pediatrics and adolescent medicine division at Johns Hopkins School of Medicine, and colleagues analyzed more than 4 million Medicaid-enrolled adolescents and learned that not only did patients most not receive post-overdose treatment, but just 1 in 54 received pharmacotherapy with buprenorphine, naltrexone, or methadone when appropriate.
Having these options for care are rendered useless if individualized treatment isn’t prioritized. Certain factors could help the prescriber determine the level of care someone needs, like whether they need to go to an inpatient treatment facility or if they are stable enough for outpatient treatment.
It’s necessary for clinicians to weigh the benefits when prescribing, especially if there are possible chances of abuse.
“There are instances where opioids are necessary,” Alinsky told HCPLive. “But as clinicians are being careful and making sure they’re only prescribing when they need to and not prescribing huge quantities, there’s definitely things that can mitigate the risk.”
The study, which focused on adolescents aged 13-22 years old, highlighted that systemic changes still need to be made to prescribing patterns.
“To me, the main takeaway is that it’s unacceptable that right now our treatment system is only able to provide the standard of care treatment to 1 in 50 youths who are coming in with an overdose—which we wouldn’t really expect for any other medical condition,” she said.
The problem won’t get fixed until prescribing providers start thinking if the overdose is part of an underlying opioid use disorder and what treatment they can help the patient access at the time. Providers must be familiar with community resources to help steer their patients in the right direction.
Where Do We Go from Here?
Incentives are also needed to have more pediatric providers prescribe such medications, by getting their waivers and targeted funding to increase the number of youth-serving addiction facilities, Alinsky concluded.The prescribing process has been laid out for providers by organizations and at the state-level, so it is important that providers have the proper information available and that insurers approve appropriate medications like buprenorphine to combat opioid abuse, Manchikanti said.
However, to reduce the number of opioid prescriptions, non-opioid techniques must be approved, including multiple interventional techniques, or new evidence-based treatment options must come to the forefront of clinical research.
Until safer, tolerable, effective pain medicine supplants the role of opioids, agencies have a responsibility to continue bettering and monitoring the means by which they reach patients today.
There’s too much at stake for them to not provide guidance.