Article
Baricitinib and Cardiovascular Events
Author(s):
Baricitinib treatment does not increase the risk for cardiovascular problems in patients with rheumatoid arthritis, according to new research.
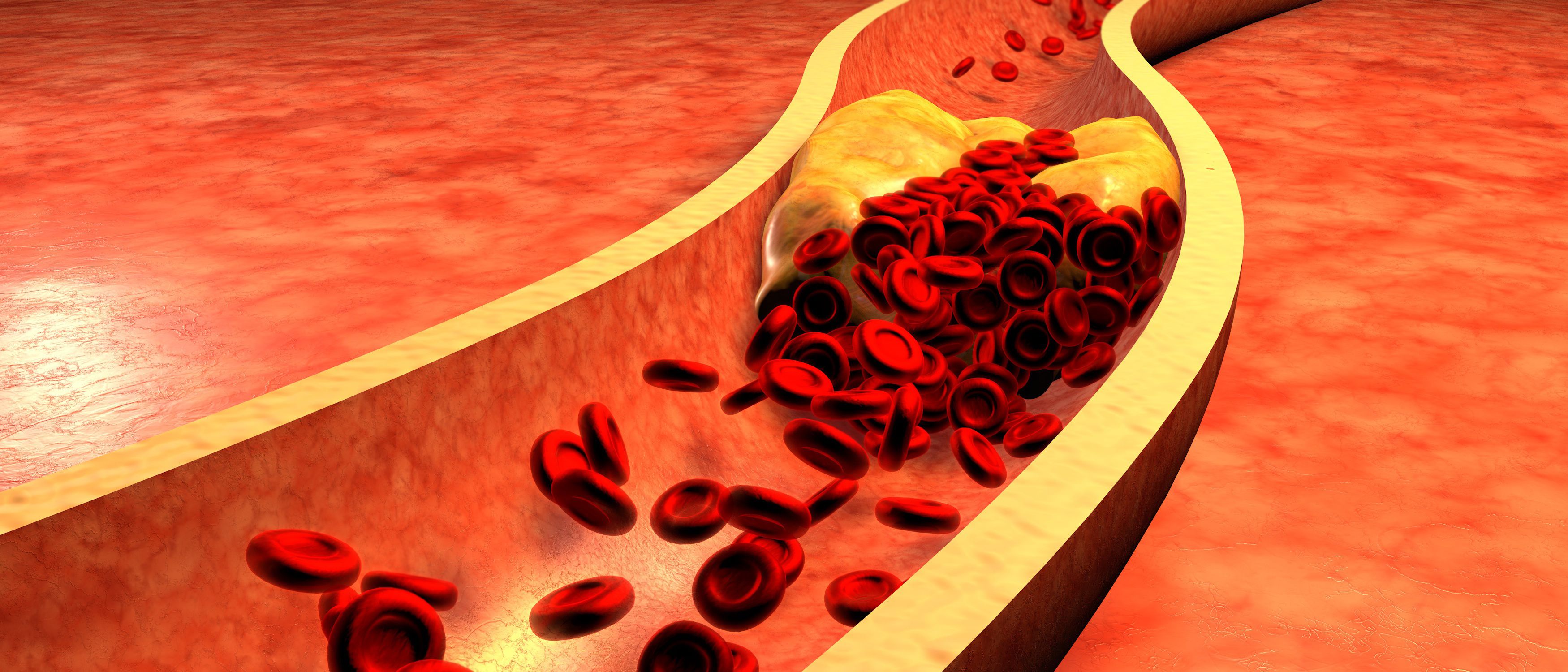
Study shows no association between baricitinib and cardiovascular events, such as arterial thrombotic events, or congestive heart failure. (©Ralwe, AdobeStock.com)
Baricitinib treatment does not increase the risk for cardiovascular problems in patients with rheumatoid arthritis, according to new research.
The study, published in a recentArthritis & Rheumatology issue, shows no association between baricitinib, an oral selective JAK1/JAK2 inhibitor, and major adverse cardiovascular events, such as arterial thrombotic events or congestive heart failure. According to investigators, these findings are important for patients who could be use this therapy long-term.
“For arterial thrombotic events and major adjudicated cardiovascular events, the frequency of reported events and incidence rates were low, comparable across treatments and analysis sets,” said lead author Peter Taylor, Ph.D., a rheumatologist at the University of Oxford. “They also did not increase with prolonged exposure.”
To determine whether the medication was linked to these cardiovascular problems, investigators analyzed data from nine placebo-controlled, baricitinib 4 mg, and baricitinib 2 mg rheumatoid arthritis studies. All total, the studies included 3,492 patients.
Study results showed the frequency of major adverse cardiovascular events didn’t increase over time and was similar between placebo and baricitinib dose groups. However, the same data revealed a small number of deep vein thromboses and pulmonary embolisms did occur during the 24-week treatment period in the baricitinib 4-mg group, but not the placebo-controlled group. Several factors, including age, body mass index, COX-2 inhibitor use, and prior history put these patients at an increased risk.
According to Taylor, the imbalance for adverse events wasn’t replicated during the treatment period for patients who switched to baricitinib 4 mg from placebo or an active comparator.
In addition, with longer-term exposure, the frequency of deep vein thrombosis and pulmonary embolism were comparable between the baricitinib 2 mg and 4 mg dose groups. The incidence rate was also stable over time among all study participants receiving baricitinib.
Ultimately, investigators said, the biological mechanistic link between JAK inhibition and increased deep vein thrombosis and pulmonary embolism remains unclear. It’s also not currently possible to identify a definitive cause-and-effect relationship. Consequently, they said, clinicians should weigh the risks and benefits when prescribing baricitinib.
REFERENCE
Taylor P, Weinblatt M, Burmester G, Rooney T, Witt S, Walls C, Issa M, Salinas C, Saifan C, Zhang X, Cardozo A, Gonzalez-Gay M, Takeuchi T, Cardiovascular Safety During Treatment with Baricitinib in Rheumatoid Arthritis. Arthritis & Rheumatology (2019), doi: 10.1002/art.40841.




