Article
Belimumab Promising as Adjunct Therapy for Lupus Nephritis
Belimumab (Benlysta, GlaxoSmithKline) can improve the kidney health of people with lupus nephritis, a new phase 3 clinical trial suggests.
(©Blueringmedia,AdobeStock)
Update December 17, 2020: The US Food and Drug Administration has approved belimumab.
Belimumab (Benlysta, GlaxoSmithKline) can improve the kidney health of people with lupus nephritis, a new phase 3 clinical trial suggests.
When combined with standard therapy, patients receiving belimumab were 60% more likely to have better kidney function, and half as likely to have kidney-related events compared to patients receiving a placebo.
Richard Furie, M.D., of the Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, in Great Neck, New York, and colleagues, reported the findings in the New England Journal of Medicine.
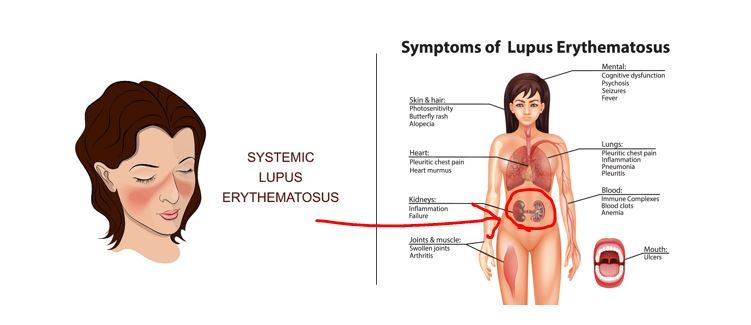
Lupus nephritis is the most common severe form of lupus erythematosus, and as many as 30 percent of patients with the condition die from kidney disease. Belimumab, a monoclonal antibody, blocks B-cell activating factor, a key mechanism of the disease.
The U.S. Food and Drug Administration approved belimumab for systemic lupus erythematosus in 2011 after phase three trials showed the drug could calm the disease. These trials excluded patients with acute, severe lupus nephritis.
But when they analyzed the results afterward, the researchers noticed that some people had protein in their urine at the start of it, an indication of kidney disease, and that the levels of the protein went down after they started taking the drug. This led them to start a new trial specifically focused on patients with lupus nephritis.
They recruited 448 people whose lupus nephritis had been confirmed kidney biopsies and randomly assigned half to receive injections with belimumab and half to receive injections with a placebo. The patients were also receiving standard treatments for lupus nephritis, and the two groups received about the same amounts of cyclophosphamide and mycophenolate mofetil. Patients tapered off their use of glucocorticoids over the course of the study.
Thirty-one patients in the belimumab group and 32 in the placebo group were black.
The researchers defined their primary end point for the study as a ratio of urinary protein to creatinine of 0.7 or less, an eGFR that was no worse than 20 percent below the pre-flare value or at least 60 ml per minute per 1.73 m2, and no use of rescue therapy for treatment failure.
After two years, 43 percent of the patients receiving belimumab met this endpoint versus 32 percent of the patients receiving the placebo, a statistically significant difference (P = 0.03).
Also 30 percent of the patients getting belimumab met the criteria of a “complete renal response” compared to 20 percent of those getting the placebo (P =0.02).
Belimumab didn’t appear to cause any serious side effects. The researchers couldn’t find any anti-belimumab anti-bodies. Six patients died in the belimumab group and five in the placebo group. And infections caused three deaths in each group.
_____________
REFERENCE
Two-Year, Randomized, Controlled Trial of Belimumab in Lupus Nephritis. Furie R, Rovin BH, Houssiau F. et al. N Engl J Med 2020; 383:1117-1128




