Article
C. difficile Is a Concern for Solid Organ Transplant Patients
Author(s):
In the past decade, the number of individuals who receive solid organ transplants has increased exponentially – something that makes the peri-transplant complications like C. Difficile a common occurrence.
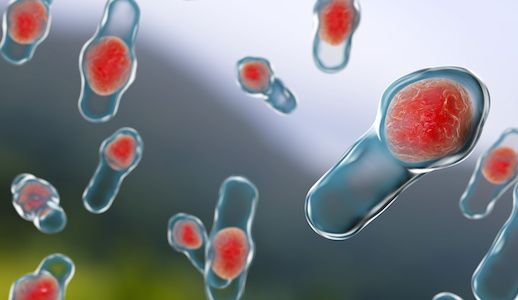
Clostridium difficile (C. difficile) infection in the solid organ transplant population carries unique risks that should be considered, according to a new literature review.
Researchers from Keck Medicine at the University of Southern California wrote a review the recent literature surrounding C. difficile infection in solid organ transplant recipients in order to further the understanding of C. difficile infection’s significant impact on morbidity and the healthcare economy of the US.
The researchers’ first major observation from the study was that antimicrobials have an enormous impact on C. difficile in solid organ transplant patients, study author Neha Nanda, MD, Hospital Epidemiologist and Medical Director of Infection Prevention & Antimicrobial Stewardship at Keck Medicine, said.
Secondly, there has not been much progress made in diagnosing C. difficile in transplant and non-transplant patients over the last decade, Nanda said.
In the past decade, the number of individuals who receive solid organ transplants has increased exponentially — something that makes the peri-transplant complications a common occurrence, according to researchers. C. difficile is just one of the complications that frequently cause morbidity in this population.
Additionally, the investigators determined through their review that fecal microbiota transplants (FMT) have shown encouraging results in the treatment of C. difficile in the solid organ transplant population. Animal studies on this topic have suggested excellent efficacy with immunization against C. difficile toxins, the study authors wrote.
Part of the way to combat the problem of C. difficile in these solid organ transplant patients requires early and accurate diagnosis of the infection in the patients, the researchers wrote.
That includes being able to differentiate between asymptomatic carriage and infection, though the “diagnostics that are currently available for C. difficile are suboptimal,” Nanda said. “Therefore, clinical judgment is imperative in making a diagnosis of C. difficile.”
The most effective method to prevent solid organ transplant recipients from acquiring C. difficile is using antimicrobials judiciously, Nanda concluded.
“Clinicians should think carefully before using antimicrobials in this population," Nanda said.
A 2014 literature review of the same topic from researchers at the Washington University School of Medicine in St. Louis, Missouri agreed that C. difficile is a significant problem in the population. Furthermore, they pointed to the emergence of a new epidemic strain, NAP1/BI/027. Even when the study was published in 2014, those researchers pointed to a lack of diagnostic tools as a major hindrance to solve the C. difficile problem in solid organ transplant patients.
A single-center study published in 2015 demonstrated that single organ transplant recipients were diagnosed with C. difficile at rates of 1.9, 7, 2.7, and 3.2 % among patients who received cardiac, lung, liver, and renal transplants, respectively. The overall C. difficile infection rate at the center was 4% throughout the 40-month study period.
The USC study, “Clostridium difficile infection in solid organ transplant recipients,” was published online in the journal Current Opinion in Organ Transplantation.
Related Coverage
C. difficile in Infancy Could Cause Allergic Diseases in Childhood
Eluxadoline Reports IBS-D Symptom Treatment Efficacy and Safety


