Article
Case Report: 52-year-old lethargic woman with nystagmus
Author(s):
A 52-year-old female with a history of diabetes, alcoholism, anxiety and major depression is brought to the emergency department for altered mental status and a possible drug overdose. What's your diagnosis?

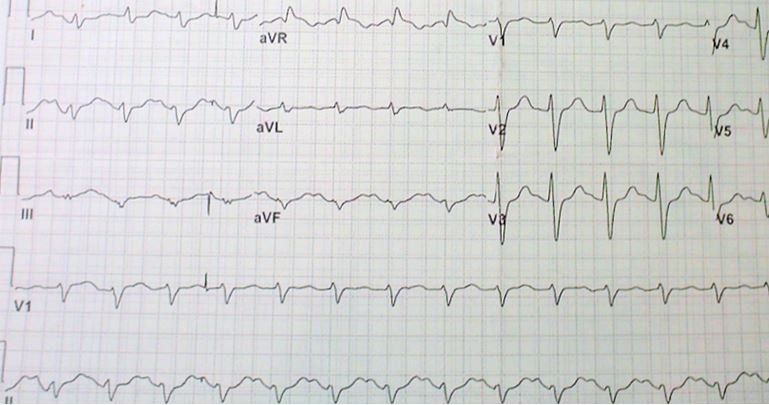
EKG read
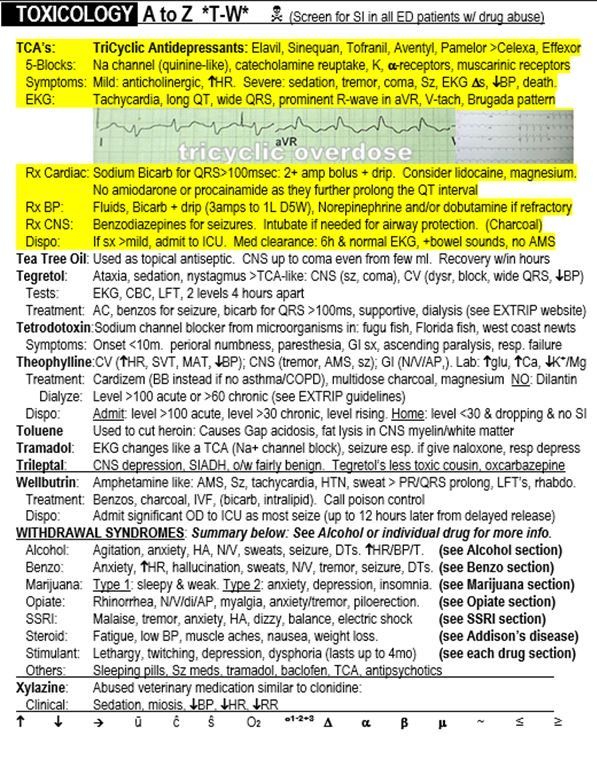
TCA overdose from "The Emergency Medicine 1-Minute Consult."
A 52-year-old female with a history of diabetes, alcoholism, anxiety and major depression is brought to the emergency department for altered mental status and a possible drug overdose. Her family believes that she has been drinking and possibly mixing alcohol with Xanax. The patient is sleepy and letting family answer all the questions. When spoken to, she won’t answer in a meaningful way. She just looks away and says, “It doesn’t matter.”
Exam: Vital signs are normal except for a pulse of ~120 and BP of 90/52. The patient is a bit lethargic and has nystagmus but is neurologically non-focal. The rest of the exam is otherwise normal.
Initial differential diagnosis: Tachydysrhythmia, Overdose, Intoxication, Alcohol withdrawal
EKG read (see image at the right):
- Sinus tachycardia
- Non-specific intraventricular conduction delay
- Right axis deviation
Do you agree with the read?
NEXT PAGE: Answer
The computer read is correct but incomplete. It does not mention the long-QT interval. For some reason I’ve noticed this occurs with alarming frequency, so I always check it myself. There is also a large R-wave in aVR. The findings in this EKG are suspicious for a tri-cyclic overdose.
CASE CONCLUSION
The patient was treated with sodium bicarb and magnesium for a possible tri-cyclic overdose and admitted to the ICU. The QRS narrowed after this. The ethanol level came back very elevated 0.325, but fortunately the Tylenol level was undetectable. A urine tox screen was positive for benzodiazepines and marijuana. (See an excerpt from the 1-minute consult on the right.)
DISCUSSION
Some of the most dangerous medication overdoses are the ones that affect cardiac conduction. Many agents can prolong the QT interval, which if severe enough can cause torsade de pointes. Calcium and beta blockers may cause bradycardia, that can progress to various types of heart block and even cardiovascular collapse. Digoxin may cause a huge variety of cardiac conduction effects. Finally, tri-cyclic antidepressants (TCAD’s or TCA’s), the culprit in this case, may cause tachycardia and prolongation of both the QRS and the QT interval that may progress to more serious conduction abnormalities including ventricular tachycardia.
TCAD’s are used less and less frequently, especially for depression, but are sometimes still used for peripheral neuropathy. Agents in the class are listed in the highlighted area of the sample page below (trade names). Celexa and Effexor are not TCAD’s but do have some similar, though milder, toxicities. Cardiovascular toxicity is primarily by sodium channel blockade, but potassium channels can also be blocked and catecholamine reuptake and muscarinic blockade likely contribute to tachycardia. Additional EKG finding not mentioned in paragraph one can include a prominent R-wave in lead aVR and a Brugada type pattern.
Treatment of cardiac toxicity from TCAD’s includes sodium bicarb for a QRS that is wider than 100 milliseconds and magnesium if the QT interval is prolonged. Lidocaine and/or electrical cardioversion is the preferred treatment for ventricular tachycardia because amiodarone and procainamide can further prolong the QT interval. For other treatment for TCAD toxicity not related to cardiac conduction see the highlighted area from the sample page below.
CASE LESSONS
- Tri-cyclic antidepressants can cause severe problems in overdose. They are rarely used for depression, but some are still used for diabetic neuropathy and a few other conditions.
- EKG findings in TCA toxicity may include any or all of the following: Tachycardia, long QT, wide QRS, prominent R-wave in aVR, V-tach, Brugada pattern
About the Author
Dr. Pregerson is chief editor of http://EMresource.org, an emergency medicine website that includes a free EM ultrasound library, EM cases of the month, EM pocket references and more.





