Article
Case Report: Asthma or Something More?
Author(s):
The latest case report from Dr. Brady Pregerson concerns a 52-year-old female with a history of asthma presenting with a cough, tactile fever, and dyspnea.
Case Report: Asthma or something more?
History: A 52-year-old female with a history of asthma presents to the emergency department for cough, tactile fever, and dyspnea. She denies syncope, palpitations, chest pain or other complaints. She states it feels like she is having an asthma attack but she hasn’t had one in over a decade so she did not have medicine for it at home.
Exam: Vital signs are notable for a pulse of 134, blood pressure of 113/62, temperature 98.6, and sat of 95% on RA. Exam is notable for obesity, tachycardia and mild wheezing but good air movement and no respiratory distress. There is no leg edema.
Initial differential diagnosis: Bronchitis, Asthma, Tachydysrhythmia, Pulmonary Embolism, Acute Coronary Syndrome.
Initial EKG
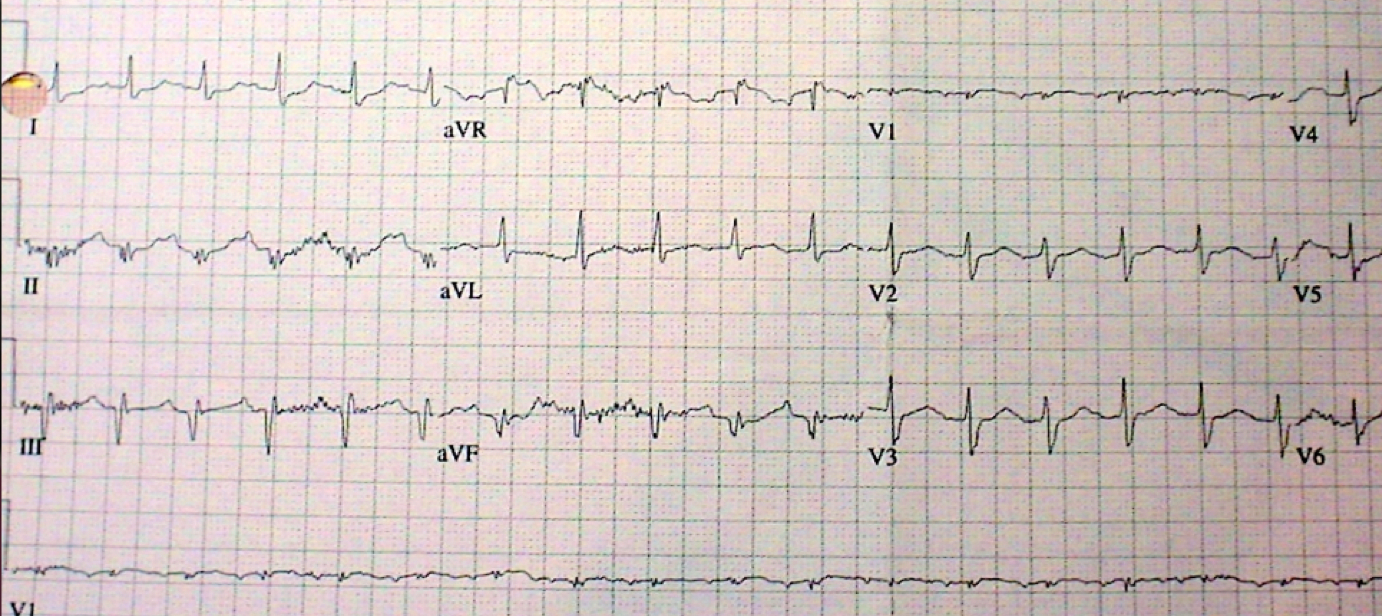
COMPUTER EKG READ:
1. Sinus tachycardia
2. Left axis deviation
3. Low voltage QRS
4. Inferior infarct, age undetermined
EKG ANALYSIS, CASE OUTCOME & 1-MINUTE CONSULT:
EKG analysis (Peer reviewed by Dr. Stephen W. Smith of Dr. Smith’s ECG Blog): The computer read is correct: the rate is >100; there is a left axis; the voltage is <10mm in all limb leads (just barely); and, there are significant Q waves in two inferior leads (III & aVF), which could, among other possibilities, represent a prior completed inferior MI. There are other possible explanations for these Q-waves of course, including a normal variant or a pulmonary embolism (incomplete S1Q3T3 without the inverted T in III). There is also fairly significant tachycardia that is not explained by pain, albuterol use, fever or other conditions, so PE, again, could be the cause. Finally, there are nonspecific T-wave changes not called by the computer.
Case Conclusion: The chest x-ray was clear with no cardiomegaly or infiltrate. Another important consideration for the differential diagnosis of low voltage and tachycardia is pericardial tamponade. A bedside echo showed no pericardial effusion (her low voltage was likely from obesity) but a possibly enlarged RV. The patient’s SOB did not improve with a trial of albuterol though her tachycardia actually ironically did improve. The WBC count was elevated at 17 with 22% bands and D-dimer was also elevated. Antibiotics were started and a chest CT was ordered to rule out PE and look for an x-ray negative pneumonia (~30% of cases of pneumonia only show up on CT, often done to check for PE). The CT showed no pneumonia but did show a saddle pulmonary embolism. The patient received half-dose tPA, was admitted and did well. No other cause of bandemia was found.
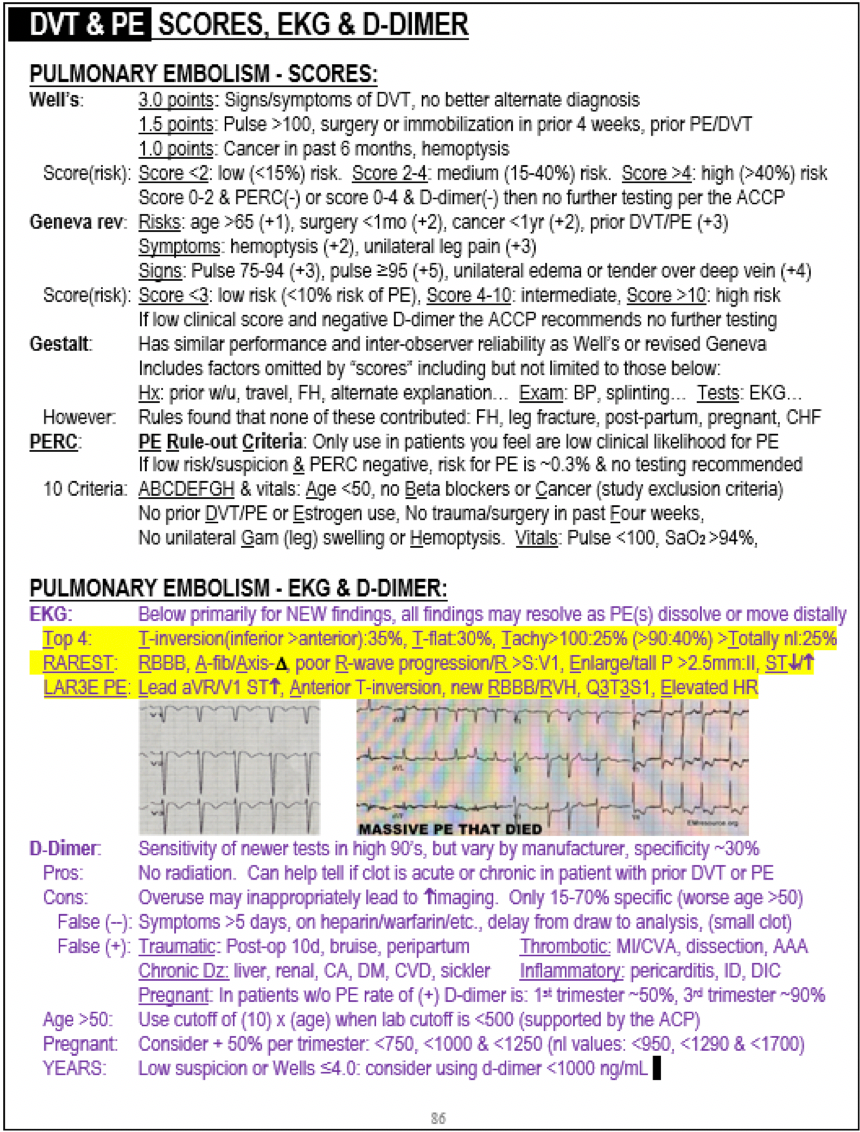
EKG in PE fromThe Emergency Medicine 1-Minute Consult
Case Lessons:
1. Consider PE with otherwise unexplained tachycardia. Though this EKG is quite nonspecific it is consistent with large PE. There will usually be other clinical findings but remember that 20% of PE’s are painless (typically the LARGE ones), and cough is present in ~1/4 of PE’s. While we are on the topic of PE and tachycardia, remember that you shouldn’t rule out PE just because there is no tachycardia as 75% of PE patients have a pulse <100 and 40% have a pulse <90.
2. Consider PE with an S wave in lead 1, especially when it is new and is in the proper clinical setting.
3. Consider PE with nonspecific T-wave changes, such as flattening, especially when they are new and are in the proper clinical setting.
4. Elevated WBC counts and even bandemia are not specific for infection.WBC is probably around 70% specific and band count around 90% specific. Any severe stress can cause demargination and elevated WBC count, not infrequently to levels >14 and occasionally to levels >30. If the cause of leukocytosis is not thought to be infectious, ordering a CRP and/or sed rate may be helpful as they will typically both be normal or if elevated only slightly so in the abscess of severe infection.
5. Conditions sometime mimic other conditions. In this case the patient felt like she was having an asthma attack, but that was unusual in that she hadn’t had one in over a decade.





