Article
Case Report: Shortness of Breath and Worsening Leg Edema
Author(s):
Our latest case report from Dr. Brady Pregerson features a man in his 40s presenting with shortness of breath and worsening leg edema. Can you determine the correct diagnosis?
History: A man in his 40’s presents to the emergency department with shortness of breath and leg edema for 2 months that has become worse during the last 2 days. He has a history of diarrhea & protein wasting due to prior gastric bypass surgery, but is otherwise healthy. He denies fever, chest pain, or cough.
Exam: Vitals are notable for tachypnea and tachycardia. He is 5’8” and weighs 258 lbs. Pulse ox is 95% on room air. The oropharynx is moist and his lungs are clear without wheezing or rales. His legs have 1-2+ bilateral edema with a negative Homan’s sign and no erythema.
EKG: Atrial fibrillation at a rate of 158 and nonspecific ST abnormalities.
Chemistry: Sodium 150, chloride 128, carbon dioxide 11, creatinine 1.7, magnesium low at 1.2, albumin low at 1.7.
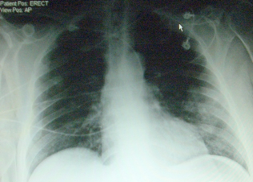
VQ scan of same patient showing perfusion defect in left lingula.

What diagnosis suggested by the X-ray?




