Article
Colorectal Cancer Study Finds Benefit From Colonoscopy Screenings
Author(s):
The slight benefit could be attributed to a lower than expected adherence to screening requests.
Michael Bretthauer, MD, PhD

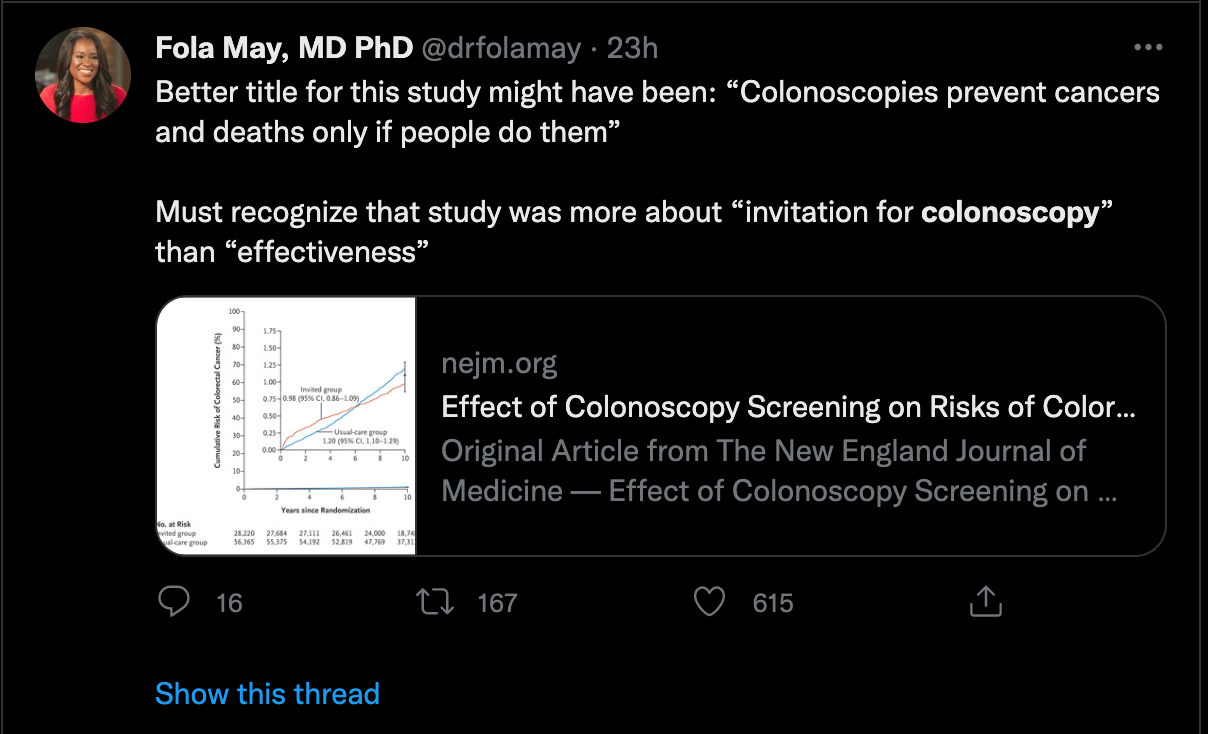
In what has become a hot debate on social media, new research shows only a small risk reduction of colorectal cancer and all-cause deaths comparing colonoscopies to usual care, likely caused by a smaller adherence to screenings than expected.
A team, led by Michael Bretthauer, MD, PhD, University of Oslo, the Clinical Effectiveness Research Group, Department of Transplantation Medicine, Oslo University Hospital, compared colorectal cancer incidence rates and deaths in patients invited for colonoscopies with patients who are not asked for a screening.
Inviting Participants for a Colonoscopy
In the pragmatic, randomized controlled NorICC trial, the investigators examined presumptively healthy individuals aged 55-64 years from population registries in Poland, Norway, Sweden, and the Netherlands between 2009-2014.
Each participant was randomly assigned to either an invitation for a single screening colonoscopy or no invitation or screening.
The investigators sought primary endpoints of the risks of colorectal cancer and related deaths, as well as secondary endpoints of death from any cause.
Overall, there was data of 84,585 individuals from Poland, Norway and Sweden, 28,220 of which were invited for a colonoscopy.
Low Colonoscopy Adherence
Of this group, 42% (n = 11,843) underwent screening. The remaining 56,365 participants were included in the usual-care group.
There were no perforations or screening -related deaths within 30 days following a colonoscopy, but 15 participants had major bleeding following the removal of a polyp.
In a median follow-up of 10 years, there were 259 cases of colorectal cancer in the colonoscopy group, compared to 622 cases in the usual-care group.
Following an intention-to-screen analysis, the risk of colorectal cancer was 0.98% at 10 years in the invited group and 0.31% in the usual-care group (RR, 0.82; 95% CI, 0.70-0.93). This represents an overall risk reduction of 18%.
In addition, the risk of colorectal cancer death was 0.28% in the invited group, compared to 0.31% in the usual-care group (RR, 0.90; 95% CI, 0.64-1.16).
The number needed to invite to undergo screening to prevent 1 case of colorectal cancer was 455 (95% CI, 270-1429).
The 2 groups had similiar all-cause death rates.
The all-cause risk of death was 11.03% in the colonoscopy and 11.04% in the usual-care group (RR, 0.99; 95% CI, 0.96-1.04).
“In this randomized trial, the risk of colorectal cancer at 10 years was lower among participants who were invited to undergo screening colonoscopy than among those who were assigned to no screening,” the authors wrote.
An Accompanying Editorial
Jason A Dominitz, MD, MHS, Division of Gastroenterology, Department of Medicine, University of Washington School of Medicine and Douglas J. Robertson, MD, MPH, White River Junction Veterans Affairs Medical Center, presented an accompanying editorial on the study in the New England Journal of Medicine.
The authors made the point that colonoscopies have been considered the predominant colorectal cancer screening tool for more than 20 years.
“However, the best evidence to support its use has been limited to data from cohort studies, which have estimated that this type of screening has been associated with a 40 to 69% decrease in the incidence of colorectal cancer and a 29 to 88% decrease in the risk of death from this disease,” the authors said. “Unlike randomized, controlled trials, which have provided support for fecal occult blood testing and sigmoidoscopy,2 cohort studies probably overestimate the real-world effectiveness of colonoscopy because of the inability to adjust for important factors such as incomplete adherence to testing and the tendency of healthier persons to seek preventive care.”
The duo went on to say the evidence gap was addressed in the NordICC study. However, they called the small risk reduction in colorectal cancer and nonsignificant reduction in the risk of death “surprising and disappointing.”
They also hypothesized as to why the results turned out the way they did. One potential reason is only 42% of participants in the NordICC trial who were invited to actually underwent a colonoscopy, compared to 58-87% in a sigmoidoscopy trial.
They also suggest the benefits of screening colonoscopy could take more time to be realized due to the fact that colorectal cancer incidence is initially increased when presymptomatic cancers are identified.
“With the use of polypectomy, the future risks of colorectal cancer and related death can be reduced if polyp resection is adequate,” they said. “The NordICC investigators plan to repeat their analysis at 15 years.”
Finally, they suggest that colonoscopy results are largely operator dependent and some participants agreed to be part of the trial and underwent screening because of an underlying concern about symptoms, which would lead to an underestimation of the per-protocol effectiveness and explain why the expected shift toward detection of earlier-stage cancer was not observed.
A Reaction From Twitter Users
Since the study was released publicly the topic of the value of colonoscopies was discussed and debated on social media among a cohort of active Twitter users in the medical community.
Vinay Prasad, MD associate professor, Department of Epidemiology and Biostatistics, University of California, San Francisco (UCSF), who has gained a massive social media following in recent months has weighed in on the study, saying flexible sigmoidoscopy is the best option as a colorectal cancer screening tool.
However, the majority of doctors weighing in on twitter have come out against this opinion, saying colonoscopies are still of value and the study had limitations that should be discussed.
The study, “Effect of Colonoscopy Screening on Risks of Colorectal Cancer and Related Death,” was published online in the New England Journal of Medicine.





