Article
A completed stress fracture in a marathon runner: Case report
This young woman sustained a hip fracture while running the Chicago Marathon. The case review suggests that training error was a critical factor. Be alert: Runners may experience stress fractures and ignore the pain.
A completed stress fracture rarely occurs in a runner competing in a marathon. However, such a fracture is a significant medical event that physicians who care for athletes should be aware of, especially when it occurs in long-distance runners who report pain in a weight-bearing bone. The risk of injury is high when athletes continue to perform a stressing activity in spite of experiencing pain, and many athletes have a high tolerance for pain and may not seek medical care. Proper diagnosis and treatment are critical to a successful outcome.
In this article, we present a case report of a woman with a completed hip fracture that she sustained while running in a marathon. Our goal is to emphasize the importance of early evaluation and management of exercise-related hip pain as well as proper exercise progression.
Materials and methods
We conducted a thorough search of the MEDLINE database for similar cases using the following search terms: femoral neck fracture/runner, stress fracture/runner, hip fracture/runner, hip stress fracture/runner, and Ritalin/bone density. No previous cases of a completed stress fracture occurring during a marathon competition were reported. The search revealed only general articles about stress fractures and 1 article about a completed fracture of the femoral neck in a long-distance runner with a diagnosis made 6 weeks after participation in a marathon.1
Case history
A 23-year-old woman trained for her first marathon in 2005 by following the Hal Higdon Marathon Training Guide (novice runner program). Five weeks into the 16-week training program, she experienced left foot pain; the clinical diagnosis was possible stress fracture.
The woman was treated with 3 weeks of relative rest. During this period, she cross-trained using an elliptical machine, cycling, and swimming. After 3 weeks, she returned to running at the 8-week level of the training program, with no graduated transition period.
At week 13 of training, the woman began to experience left lateral hip discomfort with runs longer than 12 miles. The patient self-treated with ice and acetaminophen and performed activities of daily living without pain. Her training continued uneventfully.
While running in the Chicago Marathon, the woman felt increasing left lateral hip pain at mile 17 and was unable to continue at mile 22. She was brought to the main medical tent, where she was evaluated for hip pain and was unable to bear weight. After rest and ice, the pain decreased greatly, but she was still unable to bear weight. She had no pain with passive hip range of motion or when performing an active straight leg raise test. She had some mild pain at the hip with heel percussion and with direct palpation of the lateral hip near the greater trochanter. There was no obvious swelling or bruising.
It was recommended that the woman go to an emergency department for further evaluation. However, she elected to be discharged from the medical tent non–weight bearing with crutches. She was strongly encouraged to remain non–weight bearing and to follow up in a sports medicine clinic the next morning.
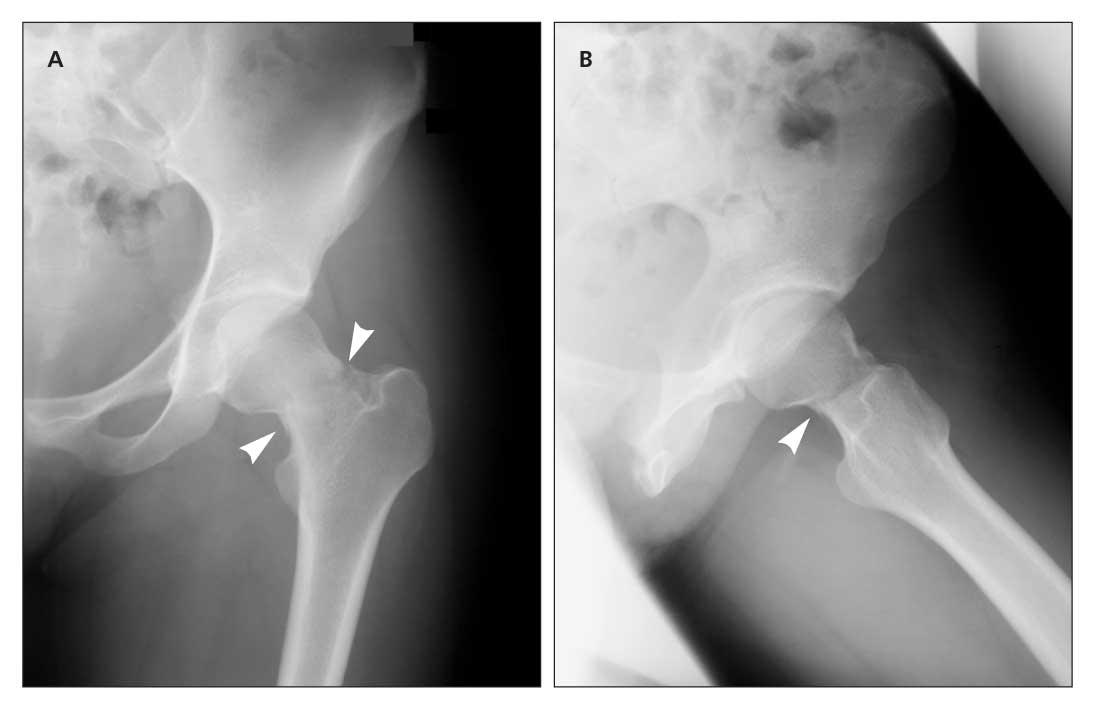
Figure – Anteroposterior (A) and frog leg (B) x-ray films show a minimally displaced femoral neck fracture (arrows).
At the clinic, the patient’s physical examination revealed an inability to bear weight and pain with active and passive range of motion. Anteroposterior and frog leg x-ray films revealed a minimally displaced femoral neck fracture (Figure). The woman was admitted for same-day surgery.
The patient’s medical history was significant for attention deficit disorder. Medications included methylphenidate used for the previous 6 years and an oral contraceptive for 5 years. Since recently discontinuing the contraceptive, she had had regular periods.
The patient reported her diet history as a balance of carbohydrate and protein, with rare carbonated beverage intake, and 2 servings of dairy per day without calcium or vitamin D supplements. She denied any history of disordered eating patterns or weight changes. During training, she reported an initial decrease in calorie intake because of poor appetite and a gradual loss of 5 lb. Her weight at the time of injury was 119 lb; her body mass index was 20.4 kg/m2.
The woman’s laboratory values were normal on admission. She underwent a left hip femoral neck closed reduction and percutaneous pinning with 3 cannulated screws without complication. A dual-energy x-ray absorptiometry (DEXA) scan obtained 2 months after the injury revealed osteopenia in her spine (T-score, −1.3; Z-score, −1.2), disuse osteopenia of the left femur, and normal bone density of the unaffected femur (T-score, −0.6; Z-score, −0.6).
Four months after surgery, additional laboratory testing performed by the patient’s primary care physician included a complete blood cell count; a chemistry panel; and measurement of serum 25-hydroxyvitamin D, parathyroid hormone, and thyroid-stimulating hormone with reflex thyroxine levels. The results of testing were normal.
The woman’s course of healing continued without incident. She was non–weight bearing on crutches for 5 weeks. During the sixth week, she started physical therapy, in which she worked on range of motion and strengthening and started a slow 3-week transition to weight bearing. At 10 weeks postoperatively, she was weight bearing as tolerated, with no hip or groin pain. She started with low-impact activities, including cycling and swimming.
At 4 months, the woman experienced no pain and had full range of motion. She progressed to walking and then to jogging on a treadmill without pain. At 8 months postoperatively, she had returned to running, with occasional mild soreness of the hip after running. She had no pain otherwise, and the results of a hip examination were normal.
Discussion
Stress fractures account for about 10% of overuse injuries and are the cause of up to 15.6% of running injuries.2 Women are 3.5 times more likely to sustain a stress fracture than men and are more likely to have a femoral stress fracture.3
Stress fractures result from repetitive microtrauma; they often are classified as insufficiency or fatigue fractures. When normal stress is placed on abnormal or osteoporotic bone, an insufficiency fracture may occur. When an abnormal amount of stress is placed on any bone-normal or abnormal-a fatigue fracture may occur.4 Bony stress reaction, a finding often seen on MRI, is part of the continuum from stress reaction to frank fracture.
Both intrinsic and extrinsic risk factors have been implicated in the etiology of stress fractures. Intrinsic factors include biomechanics (malalignment, gait abnormality, muscle imbalance, and small tibia diameter) and biochemical issues (hormonal imbalance, low bone mineral density, bone disease, and nutritional deficits). Extrinsic factors include training errors (overuse, lack of cross-training, lack of conditioning, increases in training intensity and duration, poor technique), environmental challenges (nonabsorbent training surface, banked track), and improper equipment (inappropriate footwear, prolonged use of footwear, non–gender-specific training equipment).5,6
In young, athletic women, studies relate higher stress fracture rates to a hypoestrogenic state resulting from low energy availability.7 There also is a positive correlation between menstrual dysfunction and stress fractures.2 Studies have shown a higher risk of stress fractures in female track-and-field athletes who demonstrate more restrictive eating habits.8 Although nutrition is an important factor, its role in stress fracture development is not completely understood.9
Femoral neck fractures, seen more often in women than in men, require a high index of clinical suspicion because the clinical presentation may be vague. Typical complaints include groin, thigh, or knee pain and pain with weight bearing relieved by non–weight bearing. Normal results on plain x-ray films do not exclude the possibility of a stress fracture.4
There is a greater risk of stress fractures on the tension side (superior aspect); if these fractures are not recognized and treated appropriately, they may become displaced. Displacement predisposes the patient to osteonecrosis and may result in the inability to return to sports activity at the prefracture level.10
Summary
This case report is meant to serve as a tool to provide medical professionals with information about the possibility of a completed femoral neck fracture sustained during a marathon. This may be the first reported case of a completed femoral neck fracture occurring during a marathon.
After examination of the patient’s marathon training history, we concluded that multiple factors may be associated with the development of her fracture. One significant factor is the likelihood of training error. The patient had begun training for the marathon late, with no baseline running history. In addition, she sustained a clinically diagnosed stress fracture of her metatarsal early in the training period. She was treated with relative rest and was advised to cross-train. However, after only 3 weeks of adhering to the medical recommendations, she resumed running without a gradual transition back to full training. In addition, the patient reported low calcium intake (2 servings per day) and a postinjury DEXA scan confirmed the presence of osteopenia.
This case study supports the importance of radiographic evaluation of a patient with hip and groin pain.8 If initial radiographic results are normal and there is a strong clinical suspicion of a stress fracture, further imaging (eg, MRI) should be obtained. If the patient had sought medical evaluation at the first sign of hip discomfort and early diagnosis and treatment had been initiated, this fracture most likely would have been prevented. In summary, this case report emphasizes the importance of early evaluation and treatment of exercise-related hip pain and of proper exercise progression.
References:
References1. Kerr PS, Johnson DP. Displaced femoral neck stress fracture in a marathon runner. Injury. 1995;26:491-493.
2. Marcus R, Cann C, Madvig P, et al. Menstrual function and bone mass in elite women distance runners: endocrine and metabolic features. Ann Intern Med. 1985;102:158-163.
3. Callahan LR. Stress fractures in women. Clin Sports Med. 2000;19:303-314.
4. Wall J, Feller JF. Imaging of stress fractures in runners. Clin Sports Med. 2006;25:781-802.
5. Zeni AI, Street CC, Dempsey RL, Staton M. Stress injury to the bone among women athletes. Phys Med Rehabil Clin N Am. 2000;11:929-947.
6. Dugan SA, Weber KM. Stress fractures and rehabilitation. Phys Med Rehabil Clin N Am. 2007;18:401-416, viii.
7. Beals KA, Meyer NL. Female athlete triad update. Clin Sports Med. 2007;26:69-89.
8. Bennell KL, Brukner PD. Epidemiology and site specificity of stress fractures. Clin Sports Med. 1997;16:179-196.
9. Branca F, Vatuena S. Calcium, physical activity and bone health-building bones for a stronger future. Public Health Nutr. 2001;4:117-123.
10. Clough TM. Femoral neck stress fracture: the importance of clinical suspicion and early review. Br J Sports Med. 2002;36:308-309.
Recommended readings
The authors suggest the following source for readers seeking more information:
• International Olympic Committee Medical Commission Working Group Women in Sport. Position Stand on the Female Athlete Triad. September 12, 2006. http://www.olympic.org/uk/utilities/reports/level2_uk.asp?HEAD2=1&HEAD1=1. Accessed July 21, 2008. This is a well-done and necessary position paper on the female athlete triad from the International Olympic Committee.




