Article
Continuous Intraperitoneal Insulin Demonstrates Long-term Effectiveness in Type 1 Diabetes
Author(s):
Despite intensive subcutaneous insulin therapy, a relatively small group of type 1 diabetics fails to reach adequate glycemic control, has frequent hypoglycemic episodes, or develops insulin resistance.
Most type 1 diabetes patients maintain acceptable glycemic control through subcutaneous insulin that is either injected multiple times a day or continuously infused through an external insulin pump. Despite intensive subcutaneous insulin therapy, a relatively small group of type 1 diabetics fails to reach adequate glycemic control, has frequent hypoglycemic episodes, or develops insulin resistance.
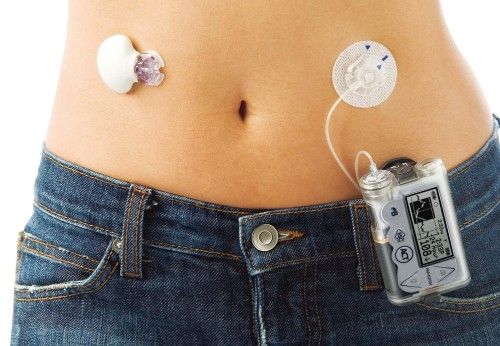
Recently, researchers in the Netherlands studied the long-term use of continuous intraperitoneal insulin infusion (CIPII) for type 1 diabetics with histories of poor glycemic control, defined as glycated hemoglobin (HbA1c) ≥7.5% and/or 5 or more incidents of hypoglycemia per week. Their research originated in 2006 as a randomized crossover study to investigate the effects of CIPII on the risk of hypoglycemia compared to intensive subcutaneous insulin treatment.
At that time, the investigators measured baseline data on glycemic control, satisfaction with treatment, and quality of life among 19 patients aged 18-70 years and then reviewed their progress after 6 months. With CIPII, they found the patients experienced improved glycemic control, treatment satisfaction, and health-related quality of life while the number of hypoglycemic events remained stable. Additionally, all of the patients chose to continue CIPII after the study concluded.
The researchers revisited the group in 2012 to assess CIPII’s long-term utility in type 1 diabetes and published the results in the April 2014 issue of BMJ Endocrine Disorders. Although using CIPII for the 6-year period produced HbA1c values equal to those associated with intensive subcutaneous therapy at the start of the study, the patients experienced significantly fewer hypoglycemic events and had greater satisfaction with their treatment. They also enjoyed a higher health-related quality of life compared to the assessments made during intensive subcutaneous therapy.
As an added benefit, CIPII produced shorter hospital admissions compared to intensive subcutaneous insulin therapy — a major factor in the increased satisfaction and quality of life measurements — and the patients experienced very few treatment-related adverse events.
Although CIPII is used as a last resort treatment for type 1 diabetes in The Netherlands, the long-term results from this small study indicate the insulin infusion may be a safe, effective, and viable treatment option for the disorder.




