Article
COPD Triples Mortality Risk in RA
Author(s):
Patients with rheumatoid arthritis have a large comorbidity burden at the time of diagnosis, including chronic obstructive pulmonary disease (COPD), asthma and interstitial lung disease, but COPD is a particular concern, say researchers writing in Rheumatology this month.
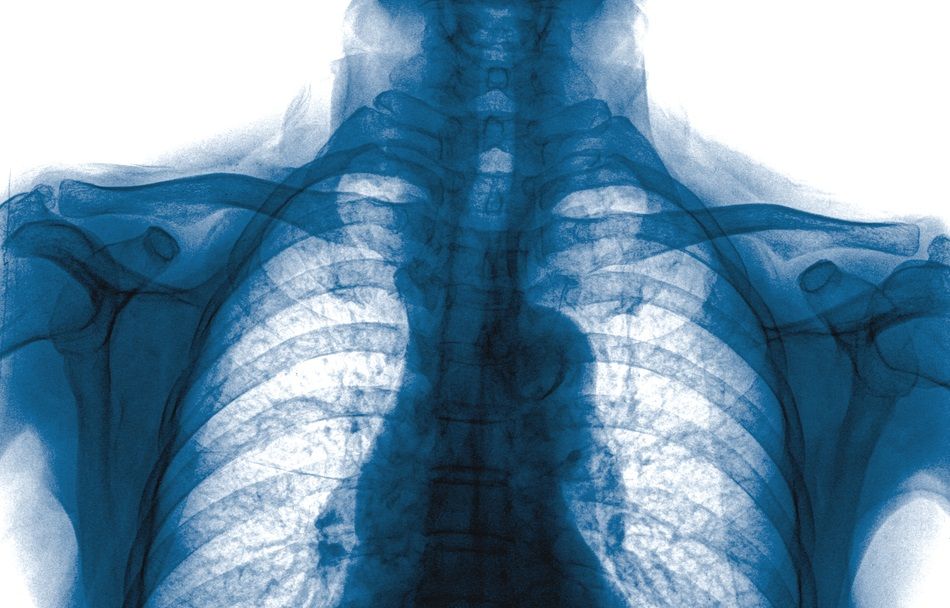
Patients with rheumatoid arthritis have a large comorbidity burden at the time of diagnosis, including chronic obstructive pulmonary disease (COPD), asthma and interstitial lung disease, but COPD is a particular concern, say researchers writing in Rheumatology this month. (©Thailoei92,ShutterStock.com)
Patients with rheumatoid arthritis have a large comorbidity burden at the time of diagnosis, including chronic obstructive pulmonary disease (COPD), asthma and interstitial lung disease, but COPD is a particular concern, say researchers writing in Rheumatology this month.
“COPD is a major predictor of early mortality in early RA,” wrote the authors, led by Karim Raza, B.M.B.Ch., Ph.D., F.R.C.P, of the University of Birmingham in the U.K. “Early assessment of comorbidity including lung disease should form part of the routine management of RA patients.”
While the long-term prognosis has improved greatly in rheumatoid arthritis with the wide use of disease-modifying antirheumatic drugs and biologics as well as a treat-to-target approach to management, mortality remains higher than in the general population, with deaths from cancer, respiratory and cardiovascular causes reported. The association between rheumatoid arthritis and cardiovascular events has been studied extensively, but there is a lack of good quality epidemiological evidence quantifying the contribution of respiratory conditions on the outcomes of rheumatoid arthritis patients.
“To our knowledge the duration between lung disease onset and RA diagnosis has not previously been explored in a community-based cohort,” the authors wrote.
This U.K. population-based study assessed the comorbidity burden in people (n = 6,591) with rheumatoid arthritis at diagnosis and early disease (three years) and its association with early mortality and joint destruction. The association between lung disease and mortality in rheumatoid arthritis was also explored. The results were compared with the same number of age- and gender-matched controls.
Respiratory disease, cardiovascular disease, stroke, diabetes, previous fracture and depression were more common (P < 0.05) in patients with rheumatoid arthritis at diagnosis than controls. Comorbidity, which was assessed using Rheumatic Disease Comorbidity Index (RDCI), was associated with all-cause mortality in rheumatoid arthritis [adjusted hazard ratio (HR) 1.26, 95% CI 1.00–1.60]. There was no association with joint destruction.
COPD, but not asthma, was associated with a near three-fold increased risk of early mortality (COPD HR 2.84, 95% CI 1.13–7.12). The sample size for interstitial lung disease was insufficient to assess for any association.
“Given the high overall mortality in people with RA the additional three--fold risk conferred by the presence of COPD is of particular importance in this group,” the authors wrote.
The excess burden of COPD and perhaps cardiovascular disease in rheumatoid arthritis patients may be related to the greater incidence of smoking observed in the participants with rheumatoid arthritis. “This underscores the importance of smoking cessation advice and support as part of the routine management of people with and at risk of RA. A holistic and patient-centric approach to the care of people with RA is vital,” the authors wrote.
The incidences of several comorbidities, including heart failure, peptic ulcer disease, depression, COPD and interstitial lung disease, were greater in the first three years after rheumatoid arthritis diagnosis than in the controls.
“Early and repeated assessment of comorbidities, including respiratory disease, should form part of the routine care of RA patients. Management of comorbidities, especially preventable and modifiable ones and associated risk factors, early on in the disease course, may improve outcomes and quality of life,” the authors wrote.
REFERENCE
Elena Nikiphorou, Simon de Lusignan, Christian Mallen, et al. “Prognostic value of comorbidity indices and lung diseases in early rheumatoid arthritis: a UK population-based study.” Rheumatology. October 3, 2019. https://doi.org/10.1093/rheumatology/kez409




