Article
CSF Biomarker Linked to Phenotype of Patients With PD
Author(s):
The findings could have implications for clinical trial subject selection and testing of symptomatic and disease-modifying therapies in PD.

Jennifer G. Goldman, MD, MS
Lower levels of cerebral spinal fluid (CSF) alpha-synuclein (a-syn) has been found to be associated with the diagnosis and motor phenotype in moderate-advanced Parkinson disease (PD), which could have implications for clinical trial subject selection and testing of symptomatic and disease-modifying therapies.
Led by Jennifer G. Goldman, MD, MS, an associate professor of neurological sciences at Rush Medical College in Chicago, Illinois, the investigators of the BioFIND study sought to explore the relationships between biomarkers for PD motor and nonmotor symptoms. To do this, the cross-sectional, observational study compared a group of patients with moderate-advanced PD (n = 115) to a group of healthy controls (n = 88).
The PD group was split into 3 subgroups based on motor phenotype as well: postural instability/gait difficulty (PGID; 36.5%), tremor dominant (TD; 51.3%), or indeterminate (12.2%).
"These associations between protein levels and clinical symptoms can help us select participants for clinical trials. For example, people with lower beta-amyloid may be more likely to develop memory problems and therefore would benefit more from a cognitive therapy,” Goldman said in a statement. “Enrolling this population in trials can help us see a treatment effect more clearly than testing the therapy on people who will not have this symptom.”
The analysis examined the relationships between a-syn within biofluids (plasma, saliva, and CSF) and other biomarkers— total tau (t-tau), phosphorylated tau (p-tau), and beta-amyloid (Aß1-42)—to the clinical features of PD. Correlations for the CSF biomarkers, as well as Movement Disorder Society-Unified Parkinson Disease Rating Scale (MDS-UPDRS) scores, motor phenotype, and Montreal Cognitive Assessment (MoCA) scores were also examined.
Results revealed that while there was no significant correlation between a-syn among the biofluids, in the CSF it was lower for the PD group (mean, 1466.25 pg/mL; standard deviation [SD], 669.20) than the control group (mean, 1713.79 pg/mL; SD, 637.16; P = .01).
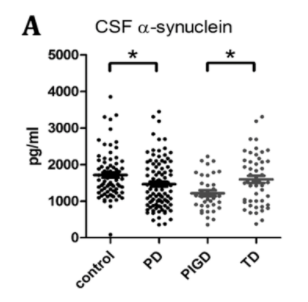
Comparisons of a-syn in CSF, in PD and healthy controls
(BioFIND)
When comparing cohorts within the PD group, it was revealed that a-syn levels were lower in the CSF of patients with PD with the PGID phenotype than those with the TD phenotype (P <.01).
Additionally, levels of t-tau (mean, 37.15 pg/mL; SD, 16.42), p-tau (mean, 16.42 pg/mL; SD, 11.10), and Aß1-42 (mean, 296.31 pg/mL; SD, 79.16) were all lower in the CSF of the PD patients compared to controls (t-tau [mean, 42.06 pg.mL; SD, 23.32], P = .08], p-tau [mean, 20.61 pg/mL; SD, 17.23; P = .05], Aß1-42 [mean, 334.75 pg/mL; SD, 89.40; P <.01]).
As expected, the PD group scored significantly lower in MoCA total scores (mean, 26.76; SD, 2.56) than the control group (mean, 27.81; SD, 1.43; P <.001) as healthy controls scoring ≤26 were excluded. MoCA remote recall (Spearman rho = .23; P = .02) and attention (Spearman rho = −.19; P = .05) subscores correlated with Aß1-42 levels for the patients in the PD group. Aß1-42 accumulates into plaques in Alzheimer disease.
"This report is an important contribution in our efforts to understand and quantify Parkinson's biology to accelerate drug development," Mark Frasier, PhD, the senior vice president of research programs at the Michael J. Fox Foundation, and an author on the paper, said. "BioFIND is a partnership between our Foundation, academia, government and—most importantly—research volunteers to measure this disease and the impact of new treatments."
The BioFIND study was supported by the Michael J. Fox Foundation, as well as the National Institute of Neurological Disorders, part of the National Institutes of Health. The study, “Cerebrospinal fluid, plasma, and saliva in the BioFIND study: relationships among biomarkers and Parkinson's disease features,” was published in Movement Disorders.





