Article
Cutaneous sural nerve injury after lateral ankle sprain: A case report
Our case report demonstrates the importance of conducting a thorough neurological examination in the evaluation of lateral ankle sprain. The patient, a dancer, reported an inversion injury to his ankle that was associated with lateral ankle pain, numbness, and paresthesia. The patient had positive Tinel test results over the distal portion of the leg in the distribution of the sural nerve. The diagnosis was a grade 1 lateral right ankle sprain complicated by an injury to the sural nerve. Treatment included scheduled anti-inflammatory medication and limited icing of the ankle. The patient returned 1 week later and reported significant improvement; after 1 month, he had returned to full activity. Knowledge of sural nerve anatomy is essential for examining physicians to make this diagnosis. (J Musculoskel Med. 2008;25:126-128)
ABSTRACT: Our case report demonstrates the importance of conducting a thorough neurological examination in the evaluation of lateral ankle sprain. The patient, a dancer, reported an inversion injury to his ankle that was associated with lateral ankle pain, numbness, and paresthesia. The patient had positive Tinel test results over the distal portion of the leg in the distribution of the sural nerve. The diagnosis was a grade 1 lateral right ankle sprain complicated by an injury to the sural nerve. Treatment included scheduled anti-inflammatory medication and limited icing of the ankle. The patient returned 1 week later and reported significant improvement; after 1 month, he had returned to full activity. Knowledge of sural nerve anatomy is essential for examining physicians to make this diagnosis. (J Musculoskel Med. 2008;25:126-128)
Injury to the sural nerve in association with lateral ankle sprain rarely is mentioned in the literature. However, this injury may occur more frequently than commonly thought, and it may be an underdiagnosed and mistreated component of ankle sprains.1
In this article, we offer a case report of a patient with sural nerve injury after ankle sprain and a discussion of the implications for diagnosis and treatment. The case demonstrates the importance of conducting a thorough neurological examination in the evaluation of the common lateral ankle sprain. We also illustrate the potential management pitfalls.
CASE REPORT
Presentation and history
A 25-year-old performer for a premier dance show reported an inversion injury to his right ankle that was associated with lateral ankle pain. Seven days later, numbness and tingling began to develop in his right heel and the lateral aspect of his right foot. When the patient was initially evaluated 11 days after the injury, he reported continued numbness in the right heel and lateral ankle region, as well as pain around the lateral malleolus. The patient had been unable to perform and was limiting his activity because of the numbness. He denied any past medical or surgical history.
Evaluation
The initial examination revealed an athletic, well-conditioned man in no acute distress but with a slightly antalgic gait. Inspection of the ankle showed mild swelling over the lateral right ankle. Palpation revealed mild pain at the anterior talofibular ligament but no pain over the calcaneofibular ligament, peroneal tendon, navicular, bifurcate ligament, base of the fifth metatarsal, or proximal fibula.
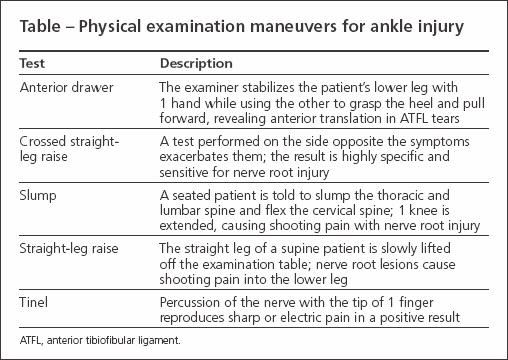
Results of the squeeze test were negative; anterior drawer testing revealed pain with stress but no laxity (Table). The patient had mild loss of range of motion of the ankle; motor testing of L3 through S1 showed 5/5 strength. The patient had positive Tinel test results over the distal portion of the leg in the distribution of the sural nerve and numbness on examination of the right heel and lateral right foot. Slump, straight-leg raise, cross-straight leg, and FABER (flexion, abduction, and external rotation) test results were negative.
Radiographs of the right ankle showed an intact mortise and no evidence of osteochondritis dissecans or acute fracture. A previous avulsion fracture was noted at the distal medial malleolus, and an anterior talar osteophyte was seen. The diagnosis was a grade 1 (mild) lateral right ankle sprain, complicated by an injury to the sural nerve.
Follow-up
Treatment involved scheduled anti-inflammatory medication and icing of the ankle for no more than 10 minutes 4 times per day. The patient was restricted in his dance to no jumping, landing, or pushing-off of the right foot. He began a home-exercise program to maintain full ankle range of motion. Bracing initially was not advised to avoid potential compression injury to the sural nerve.
The patient returned to the office 1 week later and reported significant improvement in his symptoms. He noted no pain and only mild numbness and tingling when bearing weight on the right heel. Examination results were markedly improved, with no tenderness or swelling. A Tinel test reproduced mild symptoms of heel tingling. There was mild loss of eversion at the right ankle and otherwise normal ankle motion.
The patient was permitted to return to dancing with the use of an ankle brace during performances for the following 10 to 14 days. After 1 month, the patient had complete resolution of all symptoms and had returned to full activity.
DISCUSSION
Anatomical course
The sural nerve is a purely sensory nerve of the lower extremity; its fibers originate in the S1 and S2 nerve roots.1 The sural nerve arises from the tibial nerve 3 to 5 cm distal to the knee joint in the popliteal fossa and later receives a communicating branch of the common peroneal nerve. It descends midline, between the 2 heads of the gastrocnemius muscle and becomes subcutaneous at the distal one third of the leg.2 The nerve proceeds along the lateral margin of the Achilles tendon, posterior to the lateral malleolus with the peroneal tendons, and along the dorsolateral aspect of the foot.
The anatomical course of the sural nerve corresponds to its cutaneous innervation, which includes the lateral lower third of the lower extremity, the lateral heel, and the dorsolateral aspect of the foot up to the base of the fifth toe.2 The nerve may be injured at any point along this course.
Underdiagnosed?
As a group, nerve injuries of the foot and ankle in athletes are uncommon but may be underdiagnosed.3 The sural nerve is the only nerve in the body in which the most common cause of injury is iatrogenic. Nerve grafting or biopsy of the sural nerve can cause numbness in its distribution, as well as painful neuromas at the site of damage that may require resection.
Peripheral nerve injuries
Our patient’s sural nerve neuropathy was caused by a lateral ankle sprain. The pathophysiology in this case probably involved traction to the nerve (Figure) analogous to that in traction-type injuries seen in the brachial plexus. Ensuing inflammation to the nerve itself may have resulted in our patient’s numbness and tingling.
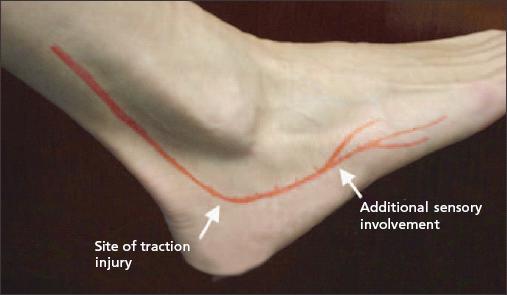
Figure –
This photograph of a healthy ankle shows the anatomy of the sural nerve, as well as the site of injury and symptoms described in this case. The course of the sural nerve corresponds to its cutaneous innervation.
Nerve entrapment–type injuries have been divided into 3 clinical stages: in stage 1, patients have pain and paresthesia at rest and at nighttime; stage 2 involves paresthesia, numbness and, occasionally, muscle weakness that occur during daytime; patients with stage 3 nerve injuries may complain of constant pain, muscle atrophy, and permanent sensory loss.1 The natural history of peripheral nerve injuries may be unpredictable.
A neurological examination of the ankle and foot always should be undertaken during the physical examination. Testing may reveal sensory deficits along the distribution of the sural nerve. The Tinel test with percussion along the course of the nerve may help delineate the location of injury and may reproduce paresthesia.
Differential diagnosis/imaging
The differential diagnosis for lateral ankle pain and paresthesia includes lateral ankle sprain, chronic ankle sprain, peroneal tendinitis, osteochondritis dissecans of the talus, fifth metatarsal fracture, lateral malleolus fracture, sinus tarsi syndrome, Achilles tendinitis, radicular symptoms referred from the lower back, complex regional pain syndrome, and sensory nerve injury involving the superficial peroneal nerve or sural nerve. Radiographs help rule out fracture, osteochondromas, and myositis ossificans as compounding diagnoses in patients who have neurological deficits.
Nerve conduction studies may be used to confirm the diagnosis when the presence of sural neuropathy is questionable; to rule out proximal nerve pathology, such as nerve root compression; or when symptoms persist. If nerve compression caused by a Baker cyst or bone spur is suspected, CT or MRI may be helpful.
Successful treatment
Our patient had a favorable outcome because the diagnosis was prompt and treatment was careful. Initial treatment should be conservative but with some considerations kept in mind. To avoid compression or thermal injury to the sural nerve, icing was limited to 10 minutes and ankle taping and bracing were not allowed until the patient’s neuropathy showed significant improvement. Scheduled NSAIDs and an initial reduction in activity were used to avoid aggravating the inflamed nerve. The patient immediately began exercises to preserve range of motion and followed with stepwise rehabilitation of his lateral ankle sprain.
A review of the literature suggests caution when patients are fitted with casts and shoes. Chronic symptoms include intractable exercise-related calf pain and prolonged numbness. These cases may involve sural nerve entrapment and require surgical neurolysis or decompression.4
Case reports also have mentioned the use of amitriptyline and clonazepam in managing pain associated with sural nerve injury. In the current case, the patient noted successful analgesia with scheduled NSAIDs.
References:
References
- 1. Hirose CB, McGarvey WC. Peripheral nerve entrapments. Foot Ankle Clin. 2004;9:255-269.
- 2. Refaeian M, King JC, Dumitru D. Isolated sural neuropathy presenting as lateral ankle pain. Am J Phys Med Rehabil. 2001;80:543-546.
- 3. Schon LC, Baxter DE. Neuropathies of the foot and ankle in athletes. Clin Sports Med. 1990;9:489-509.
- 4. Fabre T, Montero C, Gaujard E, et al. Chronic calf pain in athletes due to sural nerve entrapment: a report of 18 cases. Am J Sports Med. 2000;28:679-682.




