Determining treatment of lumbar disk protrusion and disk extrusion
Author(s):
Disk herniation is a common spine disorder that has a wide range of presentations and clinical significance.1,2 The potential for recovery varies from patient to patient, depending on the size of the protrusion, the size of the canal, the patient’s age and activity level, and the extent of disk disruption.3
Disk herniation is a common spine disorder that has a wide range of presentations and clinical significance.1,2 The potential for recovery varies from patient to patient, depending on the size of the protrusion, the size of the canal, the patient’s age and activity level, and the extent of disk disruption.3 Often, radiologists use vague terms to describe the herniation, and the literature is not helpful in characterizing what types of herniations are likely to benefit from what kinds of treatment. Because different forms of herniation may represent both a different aspect of disk deterioration and a different indication for treatment, comparisons can help physicians understand the relative indications for surgery.
This single case study demonstrates the differing clinical presentations that determine treatment of lumbar disk protrusion and disk extrusion. In this article, I describe the case of a patient who presented with a bulging disk and then later with disk extrusion. I discuss the principles that guide proper treatment and offer an algorithm for a conservative exercise program.
CASE PRESENTATION
Bulging disk
A 38-year-old man first presented to the spine clinic for evaluation of herniated nucleus pulposus (HNP) after his local physician obtained an MRI scan of his lumbar spine. The patient was in excellent health, a nonsmoker, and fully employed at a job that involved frequent lifting and trunk twisting. About 6 months before his referral, he had begun to experience episodic and then more persistent low back pain (LBP) that often became severe at the end of the day. He found that bending and twisting aggravated the LBP symptoms and that prolonged sitting was becoming painful as well.
Within the previous 2 months, the man had begun to notice unilateral leg pain symptoms running down the back of his calf to the foot; the symptoms were associated with the same activities that aggravated his back pain. Occasionally, the symptoms were intense, but not as intense as his worst back pain.
The patient considered his LBP to be 70% of his problem and his leg pain 30%. At its worst, his LBP rated an 8 on a 10-point scale; his leg pain rated a 6. He was modifying the way he did his work. He had missed a few days but was in no danger of losing his job. He had seen some improvement with the use of NSAIDs that his primary care physician prescribed, but he had not started a physical therapy program, because MRI findings showed a disk herniation.
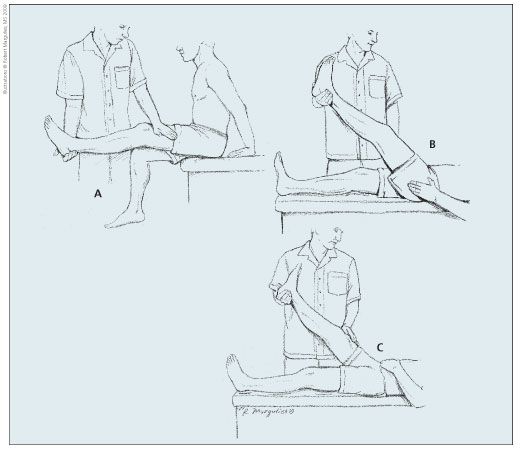
Figure 1 –Performing a straight-leg raising test with the patient in the sitting position (A) provides the physician with a means of validating the patient’s subjective report of radicular pain during the more familiar supine straight-leg raising examination (B). The test is sensitive for disk herniation, and patients with nerve root compression should experience similar symptoms in both positions. In the contralateral straight-leg raising test (C), elevation of the nonpainful leg triggers radicular pain in the symptomatic limb; this test is highly specific for disk herniation. Results of these tests are not considered positive unless pain radiates distal to the knee in the distribution of the involved L5 or S1 nerve roots.
At this point, the findings on the patient’s examination were rather benign. He had excellent strength and sensation in both lower extremities, although he complained of some numbness over the lateral aspect of his left calf. A straight-leg raising test was performed (Figure 1). The results were normal, although some back and buttock pain was elicited. The patient’s reflexes were normal, but range of motion in his back was reduced to half of normal because of lumbosacral back pain. He made an excellent effort and was able to push through the back pain to improve his motion.
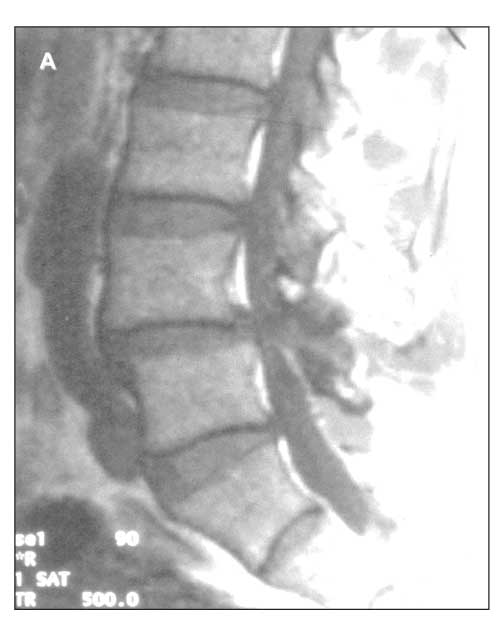
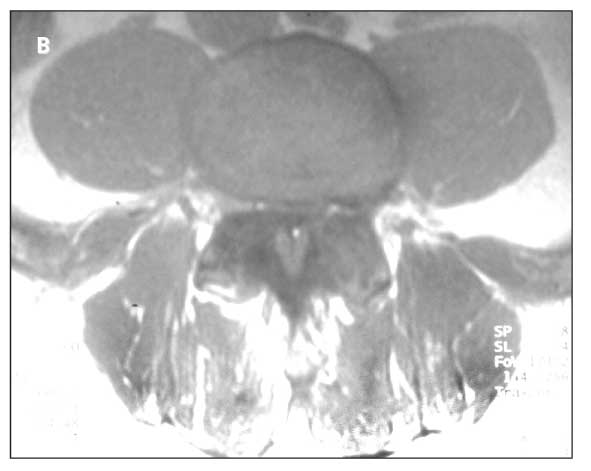
Figure 2 –A sagittal MRI scan (A) obtained at the patient’s initial presentation shows a narrow canal, a broad-based disk bulge, and a small amount of L4-5 spondylolisthesis. There is no focal herniation, although the anulus impinges on the thecal sac. This axial MRI scan (B) demonstrates a broad-based bulge; there is no focal herniation of nuclear material or focal nerve root compression.
MRI demonstrated a broad-based disk protrusion that was eccentric to the left and was compressing the thecal sack and the nerve root at L4-5 on that side (Figure 2). The disk was dark, revealing desiccation, but maintained good overall height. There was no evidence of an extruded or free fragment of the
disk associated with the herniation. Although a low-grade spondylolisthesis suggested degeneration of the disk, no other abnormalities were seen.
Because the patient had good motor function, a lack of tension signs, and mild to moderate neural compression, he was encouraged to proceed with the physical therapy program that had been prescribed by his primary care physician.4 After the patient performed range of motion exercises and back and abdominal strengthening exercises and had training in lifting and activity techniques (Table), his LBP improved significantly and his leg pain resolved. The patient adopted an aerobic exercise program and returned to work without further impairment.
Herniation
Ten months later, the patient returned to the spine clinic; he had slipped and fallen while working at home. Now his symptoms were dramatically different. His LBP was severe again-rating an 8 out of 10-but his leg pain was exquisite, rating 10 out of 10 (“if not worse”) and representing 90% of his pain concerns. His symptoms had not abated with 10 days of conservative treatment, including the use of NSAIDs and analgesics, and he felt unable to continue any activity because of his current level of pain. He was comfortable only when reclining with his knees flexed and could neither stand nor lie flat without experiencing severe pain in the posterolateral calf and foot. Intolerable pain was triggered by any change in position and any increase in activity.
Examination revealed weakness of the gastrocsoleus muscle group, weakness of the tibialis anterior, and effort-related weakness of the quadriceps and hamstrings, all on the left side. A left-sided straight-leg raising test reproduced severe distal leg pain at 20°, and a contralateral (right-sided) straight-leg raising test elicited the same symptoms at 35°. The radicular symptoms were aggravated at less than 45° of elevation with both ipsilateral and contralateral testing, signs that are sensitive and specific for nerve compression by an HNP. Deep tendon reflexes, previously normal throughout, revealed a significant loss in the left ankle jerk reflex. Bowel and bladder function remained intact.
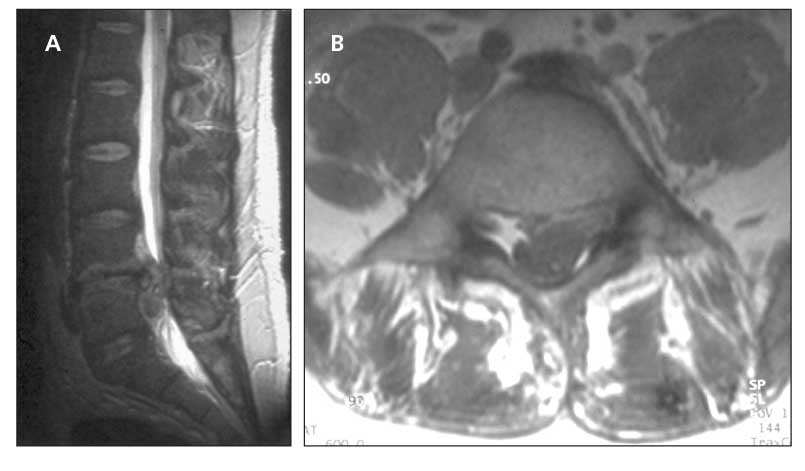
Figure 3 –This sagittal MRI scan of the patient was obtained post disk extrusion (A). The thecal sac is grossly displaced dorsally against the lamina by the large herniated nucleus pulposus. The normal column of cerebrospinal fluid is not present at the level of compression, and epidural fat has been displaced. This axial MRI scan shows the large, focal extrusion displacing the entire thecal sac dorsally and to the right (B). The posterior longitudinal ligament has been elevated away from the outer anulus at the margins of the herniation.
A repeated MRI scan revealed a large disk extrusion that was compressing the entire thecal sack and left-sided nerve roots at L4-5 (Figure 3). The entire nucleus pulposus had extruded through the anulus fibrosus beyond the extremes of the previous annular bulge. Epidural fat seen on the previous MRI scan, a sign of residual space available to the nerves, was displaced from the zone of compression; the cerebrospinal fluid that typically fills the thecal sack at the lumbar level also was absent. The patient’s symptoms and disability were extreme. In many patients, large herniations resorb5; however, this patient was unable to tolerate his severe radicular pain despite being completely inactive and taking narcotic analgesics. And although the patient had been comfortable with the idea of receiving nonoperative care when back pain was his biggest problem, he was desperate for surgery when he returned with leg pain. After the options and risks were discussed in detail, he was eager to proceed with the surgery.
Surgical treatment was carried out to remove the extruded fragment, which was as extensive intraoperatively as it appeared on the MRI scan. The disk space was found to have extruded all of the nuclear material, and the segment had become highly unstable; these findings warranted the somewhat uncommon addition of an interbody fusion to maintain spinal alignment and relieve the patient’s baseline back pain.
The patient experienced immediate relief of his leg pain and return of normal strength and sensation. His LBP was reduced to its preinjury level. After an appropriate period of recovery and rehabilitation (3 weeks of limited activity; 3 weeks of increased activity at home; progressive physical therapy until 3 months postoperative, awaiting fusion at the L4-5 level), the patient was able to return to unrestricted work and recreational activities.
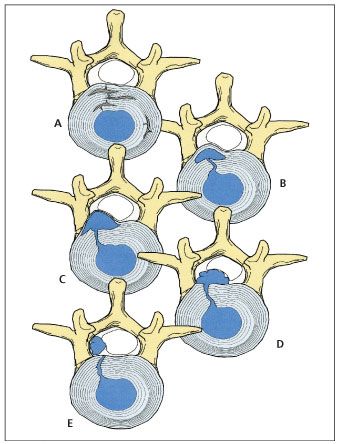
Figure 4 –Different terminology and criteria are used for defining the extent of disk herniation seen on MRI. Classification of herniated nucleus pulposus (HNP) as applied in the lumbar spine is as follows: disk bulge resulting from degeneration (A); HNP protrusion (B); extruded HNP, subligamentous or contained (C); extruded HNP, uncontained (D); sequestered HNP, free fragment (E).
DISCUSSION
Three principles can help guide proper treatment of patients with lumbar disk disorders.6-9 First, MRI observations of disk degeneration and herniation are poorly correlated with clinical signs and symptoms; the patient history and examination are the best guide to treatment. Second, annular bulges associated with disk degeneration and disk-space narrowing are physiologically and clinically distinct from protrusions and extrusions of nuclear material that result from true herniation. Third, different readers may use different terminology and criteria for defining the extent of herniation seen on MRI. Less quantifiable terms, such as “massive,” “extensive,” “bulging,” and “significant,” should be avoided in favor of more quantifiable terms, such as “extruded,” “contained,” and “subligamentous.” The treating physician should view MRI studies personally or review and discuss them directly with the radiologist. The physician should apply objective criteria to the interpretation before he or she embarks on treatment (Figure 4).
Even a “large” extruded disk may be clinically tolerable if the canal is likewise large and the nerve roots are minimally effaced and not compressed. At the same time, a focal, contained, subligamentous herniation may produce severe symptoms if it occurs in the foramen adjacent to the dorsal root ganglion of the affected nerve. Clinical examination, repeated over time, often yields the best prediction of recovery and relief with nonoperative care. Repeated examination also identifies patients whose symptoms result from significant nerve root compression and who may require surgical care.10
References:
References1. Garfin SR, Rydevik BL, Brown RA. Compressive neuropathy of spinal nerve roots: a mechanical or biological problem? Spine. 1991;16:162-166.
2. Ljunggren AE, Jacobsen T, Osvik A. Pain descriptions and surgical findings in patients with herniated lumbar intervertebral discs. Pain. 1988;35:39-46.
3. Thelander U, Fagerlund M, Friberg S, Larsson S. Straight leg raising test versus radiologic size, shape, and position of lumbar disc hernias. Spine. 1992;17:395-399.
4. Weber H. Lumbar disc herniation: a controlled, prospective study with ten years of observation. Spine. 1983;8:131-140.
5. Saal JA, Saal JS, Herzog RJ. The natural history of lumbar intervertebral disc extrusions treated nonoperatively. Spine. 1990;15:683-686.
6. Boden SD, Davis DO, Dina TS, et al. Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects: a prospective investigation. J Bone Joint Surg. 1990;72A:403-408.
7. Ljunggren AE. Natural history and clinical role of the herniated disc. In: Wiesel SW, Weinstein JN, Herkowitz HN, et al, eds. The Lumbar Spine. Philadelphia: WB Saunders; 1996:473-491.
8. Thornbury JR, Fryback DG, Turski PA, et al. Disc-caused nerve compression in patients with acute low-back pain: diagnosis with MR, CT myelography, and plain CT [published correction appears in Radiology. 1993;187:880]. Radiology. 1993;186:731-738.
9. Urban LM. Straight-leg-raising test: a review. J Orthop Sports Phys Ther. 1981;2:117-133.
10. Wood EG, Hanley EN. Lumbar disc herniation and open limited discectomy: indications, technique and results. Operative Tech Orthop. 1991;1:23-28.





