Article
Diabetic Retinopathy May Predict Hemodialysis Induction in Patients with T2D
Author(s):
Diabetic retinopathy and microalbuminuria were associated with a significantly higher risk of hemodialysis induction in individuals with T2D.
Credit: Adobe Images
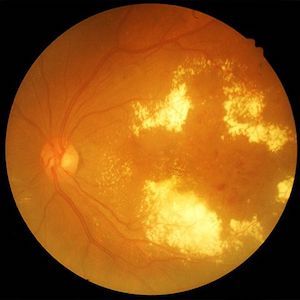
New research suggests diabetic retinopathy is predictive of hemodialysis induction in patients with type 2 diabetes (T2D) at the early stage of diabetic nephropathy, with normo- and microalbuminuria and normal renal function.1
The results, presented at the 83rd Scientific Sessions of the American Diabetes Association (ADA 2023), indicate microalbuminuria is a risk factor for hemodialysis induction and diabetic retinopathy is a more predominant predictor for hemodialysis at the early stages of diabetic nephropathy.
“Proliferative diabetic retinopathy is a risk factor for hemodialysis induction even in normoalbuminuria subjects with normal renal function,” wrote the investigative team, led by Tatsumi Moriya, of the health care center at Kitasato University.
Moriya and colleagues stressed the importance of elucidating which factors are associated with the progression of diabetic nephropathy toward end-stage renal disease, as early a stage as possible.2 The team hypothesized that different grades of diabetic retinopathy affect the progression toward hemodialysis in individuals with T2D with normoalbuminuria or microalbuminuria, and normal renal function.1
A total of 2478 outpatients with GFR measured by iohexol injection between 1995-2013 and ≥5 years of follow-up were analyzed by the investigative team. After exclusions, a total of 448 patients with type 2 diabetes and normal renal function (estimated glomerular filtration rate [eGFR] ≥60 ml/min/1.73 m2) were followed-up with for the analysis. In the population, 278 patients have normoalbuminuria and 170 patients had microalbuminuria.
At baseline, the investigative team divided HbA1c levels into HbA1c ≥7.0 (n = 327) and <7.0 (n = 121) groups. A total of 86 participants had simple diabetic retinopathy and 65 had proliferative diabetic retinopathy, and 217 had hypertension. Participants were followed-up with for an average of 16 years. The main study outcome was hemodialysis induction, while the risk of developing hemodialysis induction was evaluated using Kaplan-Meier analysis.
Over the study period, a total of 7 subjects with normoalbuminuria and 11 subjects in microalbuminuria began to receive hemodialysis. The Kaplan-Meier analysis suggested that diabetic retinopathy (Wilcoxon, 5.82; P = .016), proliferative diabetic retinopathy (Wilcoxon, 8.53; P = .014), and microalbuminuria (Wilcoxon, 5.87; P = .015) were associated with a significantly higher risk of hemodialysis induction than no diabetic retinopathy, simple diabetic retinopathy, and normoalbuminuria, respectively. Investigators noted neither HbA1c nor hypertension were associated with the risk of hemodialysis induction.
On multivariate analysis, diabetic retinopathy (P = .042), but not microalbuminuria, was significantly associated with hemodialysis induction in all participants. Within each group analysis, Kaplan-Meier analysis revealed that proliferative diabetic retinopathy was associated with hemodialysis induction in normoalbuminuria. Meanwhile, simple diabetic retinopathy and proliferative diabetic retinopathy were not associated with hemodialysis in microalbuminuria and HbA1c or hypertension did not affect hemodialysis in either group.
“Microalbuminuria itself is a risk factor of hemodialysis induction at the early stage of diabetic nephropathy (normo- and microalbuminuria with normal renal function),” investigators wrote. “The prepro-proliferative diabetic retinopathy is a risk factor for hemodialysis induction even in subjects with normoalbuminuria and normal renal function.”
References
- Moriya T, Suzuki A, Hayashi A, Matsubara M, Miyatsuka T. Diabetic Retinopathy Predicts Hemodialysis Induction in Subjects with Type 2 Diabetes with Normo- and Microalbuminuria and Normal Renal Function. Poster presentation at the 83rd Scientific Sessions of the American Diabetes Association. June 23 – 26, 2023.
- Diabetic nephropathy - statpearls - NCBI bookshelf. National Library of Medicine. Accessed June 30, 2023. https://www.ncbi.nlm.nih.gov/books/NBK534200/.





