Article
Diagnosis and Management of Complex Regional Pain Syndrome
Complex regional pain syndrome (CRPS) can be tricky todiagnose. This review describes criteria for identifying CRPS, and gives guidance for treatment, with case studies and photographs.
ABSTRACT: Complex regional pain syndrome (CRPS) can be tricky to diagnose. The International Association for the Study of Pain established criteria that differentiated CRPS as type 1 (formerly called "reflex sympathetic dystrophy") or type 2, associated with nerve injury (formerly called "causalgia"); patients also had to have pain disproportionate to the inciting event. Newer, stricter criteria have been proposed that cluster signs and symptoms and require documentation of objective findings as well as symptoms reported by the patient. The key to identifying CRPS is to obtain a proper history, document objective findings, and rule out other disorders that can imitate the condition. Treatment tends to be multifaceted; it includes physical mobilization of the affected limb and medications to help alleviate discomfort. (J Musculoskel Med. 2008;25:464-469, 490)
Silas Weir Mitchell (1829-1914) described "causalgia" after nerve injury during the American Civil War. Over time, the syndrome was given multiple and colorful names, such as algodystrophy, sympathalgia, and posttraumatic spreading neuralgia. The term "reflex sympathetic dystrophy" (RSD) attributed to Evans in 1946 referred to a clinical syndrome similar to that observed in causalgia but in the absence of overt nerve injury. Both entities were renamed "complex regional pain syndrome" (CRPS) at the Orlando consensus workshop in 1993, and new criteria were adopted in 1994 by International Association for the Study of Pain (IASP) taxonomy.1

Figure 1
– Swelling is seen in the right leg
of a patient with complex regional pain
syndrome type 1.
The criteria described CRPS type 1 (formerly known as RSD) and type 2 (formerly known as causalgia) as syndromes (a) arising after an initiating noxious event in the absence (CRPS 1) or the presence of overt nerve injury (CRPS 2); (b) with spontaneous pain or allodynia/hyperalgesia not limited to the territory of a single peripheral nerve (for CRPS 1) and disproportionate to the inciting event; (c) with past or present evidence of edema, skin blood flow abnormality, or abnormal sudomotor activity; and (d) excluding other conditions that would otherwise account for the degree of dysfunction.
This taxonomy was meant to be descriptive and general rather than implying etiology or pathophysiology.1 It acknowledged that in some cases the sympathetic nervous system (SNS) may be involved, but the mandatory and all-inclusive role of SNS was minimized. In this article, we discuss the diagnosis and management of CRPS, with emphasis on CRPS 1.

Figure 2
– In a patient with recalcitrant complex
regional pain syndrome type 1 (photograph taken
while the patient was under general anesthesia),
fixed dystonic posturing was established within
3 months even though sympathetic blocks,
opioid analgesics, neuropathic medications,
and aggressive therapy were used.

Figure 3 – A patient with complex regional pain syndrome type 1 had fixed posturing associated with coldness and profound allodynia 1 year after injury (A). The patient had been immobilized inappropriately in the "position of comfort" early after injury without much therapy to mobilize the extremity (B).

Figure 4 – A patient with complex regional pain syndrome type 2 has a lateral plantar nerve laceration (A). Widespread severe allodynia has resulted in dry scaly skin because the patient has been unable to wash the foot for 1 year (B).
Current state of knowledge
The syndrome continues to perplex, fascinate, and frustrate clinicians and researchers alike. Although very sensitive, the 1994 criteria lacked specificity and led to over diagnosis of CRPS type 1.1 Given the high false-positive rate of IASP criteria, a combination of symptoms and signs were proposed by Harden and Bruehl2 to increase discrimination between CRPS and non-CRPS patients.
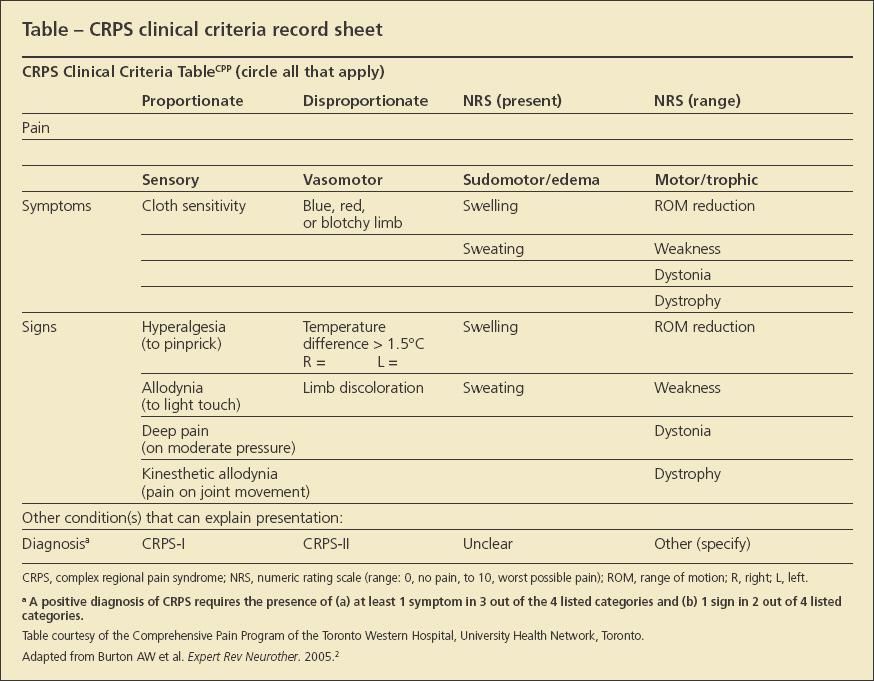
These criteria were published in an IASP-sanctioned book but are not formally adopted yet. The new criteria proposed that the patient must not only have pain disproportionate to the inciting event but also report 1 symptom in 3 of 4 categories (sensory, vasomotor, sudomotor/edema, and motor/trophic) and display at least 1 sign in 2 or more of the above 4 categories. These criteria cluster categories of signs and symptoms that have been proved meaningful by research introduce a separate category of motor problems (paired with trophic changes). The accompanying Table (see below) has been created on the basis of these criteria and is currently in use by our own pain program, the Comprehensive Pain Program of Toronto Western Hospital.
However, we caution that the current proposed criteria as well as the 1994 IASP classification have great difficulty accounting for patients who present with large areas of hypoesthesia instead of hyperesthesia (personal communication with Norman Harden, coauthor of the Harden and Bruehl criteria). Such hypoesthesia is not rare and seems to be a central phenomenon but is poorly understood.3
At present, CRPS type 1 is considered to be a multifactorial regional syndrome.4 It affects both the peripheral nervous system and CNS and additionally has musculoskeletal, endocrinological, and vascular ramifications.
The incidence of CRPS type 1 in the general population is reported by Sandroni and associates5 to be 5.46 persons/100,000 with period prevalence (1989-1999) of 20.57/100,000. Women are affected 4 times more often than men. Approximately three-fourths of CRPS type 1 cases in the community resolve spontaneously, while pain clinics address refractory CRPS. In another study, however, the incidence was recorded to be 4 times higher than the one reported by Sandroni and colleagues.6
Diagnosis
There is no gold standard for diagnosing CRPS type 1. However, it is the examining physician's responsibility to obtain as much objective evidence as possible and make sure other conditions are excluded (Figures 5 through 7).
The cornerstone of diagnosis lies with a detailed history and a thorough physical examination. Given the overdiagnosis of CRPS type 1 by the generous 1994 IASP criteria (which are often applied without excluding other disorders that can imitate CRPS),1 we strongly recommend the stricter criteria proposed by Harden and Bruehl,2 even if they have not been formally adopted yet by the IASP. The accompanying Table can serve to tabulate self reported symptoms (by the patient) and document signs observed by the clinician at the time of consultation. Harden and Bruehl outlined for the interested reader the clinical application of the newly proposed criteria and the most recent concepts about CRPS subtypes.

Figure 5 – Patients often are referred for having complex regional pain syndrome (CRPS) type 1 but prove to have another condition. A CRPS 1–like presentation resulting from complete immobility and limb dependency secondary to "fear of movement" in the presence of widespread hypoesthesia is shown (note that hyperesthesia is expected in CRPS). Intense mobilization and range of movement resulted in a dramatic reduction of swelling and discoloration.

Figure 6 – A CRPS 1–like presentation is shown (A). Note the ligature sign at the elbow in a patient with a factitious disorder (B).
In regards to common diagnostic tests available to the practicing clinician, the following should be noted:
• Although the 3-phase bone scan historically has been regarded as important in support of the diagnosis of CRPS types 1 and 2, several studies have cast doubts as to its veracity. It is recommended that a bone scan consistent with CRPS (typical periarticular uptake in the delayed phase) not be considered equivalent to having the syndrome, because such scans have been observed after sympathectomy, in abnormal weight-bearing use of an extremity, in completely asymptomatic persons, or even in factitious disorders.7
Clinical judgment is necessary to make the connection between the scan and the diagnosis. The absence of such a bone scan in our view does not exclude the entity, particularly months after the onset. Similarly, in our view, a positive bone scan result does not confirm the disorder unless it corroborates appropriate symptoms and signs as discussed above.
• Sympathetic blocks have shifted from a "diagnostic" test to a therapeutic procedure that can enhance and facilitate uncomfortable physical therapy. The concept of "sympathetically maintained pain" has lost its previous significance as CRPS-related mechanisms may shift and change over time. The response to sympathetic blocks should not be used to make the diagnosis.8
• Osteopenia seen in a plain x-ray film could be the result of intense immobilization alone. However, rapid onset of significant osteopenia after a trivial injury in the presence of serious pain and other signs and symptoms, such as those listed in the Table, should at least alert the physician to the syndrome as a part of the differential diagnosis.
• Electromyographic and nerve conduction studies can rarely be tolerated in the presence of allodynia and hyperalgesia, and results are negative in CRPS 1. Their value lies only in confirmation of CRPS 2.
• MRI of the involved limb may show bone marrow signal changes; thermography does demonstrate temperature differentials between the involved and uninvolved limbs.
All the tests reported here serve as adjuncts to the diagnosis of CRPS 1. In our opinion, however, they cannot replace the important triad of (1) history, (2) objective documentation of abnormalities, and (3) exclusion of other disorders (disease imitators).

Figure 7– A patient was referred for having bilateral complex regional pain syndrome type 1 of spontaneous origin after an acute onset of bilateral leg lesions, severe allodynia, and swelling. Skin biopsy results revealed Degos disease, a rare autoimmune disease associated with peripheral skin lesions and small-fiber neuropathy.
Management
A series of recent articles on the nature and management of CRPS unanimously concluded that "functional restoration is the necessary and often sufficient condition "to restore health; other treatments serve primarily to facilitate this.2 We consider that CRPS type 2 is easier to diagnose, given the presence of overt nerve injury that can be documented electrophysiologically or during surgical exploration. CRPS type 1 seems, however, to be surrounded by controversy.
On the basis of the most recent concept that CRPS in general is a multifaceted disorder, its care must indeed be multidimensional.4 Mobilization of the involved limb as early as possible is the cornerstone of treatment to avoid permanent changes in the peripheral nervous system and CNS. This should include range of movement and stress-loading techniques. At the same time, pain control (oral and via sympathetic blocks, if the patient responds to them) is of paramount importance to allow for mobilization.2
Although combined approaches seem more effective than single modality treatments for all forms of chronic noncancer pain, including CRPS, interdisciplinary pain rehabilitation programs may be required for patients with intractable pain. These treatments typically provide education; reconditioning physical/occupational therapy; a pharmacological approach; biofeedback/relaxation training; operant conditioning; psychotherapy (personal and family); treatment of psychiatric comorbidity; and interventional approaches, such as nerve blocks, spinal cord stimulation, and intraspinal analgesia.
In pharmacological approaches, the only evidence-based preventive strategy for CRPS is the use of vitamin C (200 mg/d) in patients who have sustained wrist fractures.9 For therapy in established CRPS, the literature suggests the following therapeutic approaches:
• A short course of oral corticosteroids can be of value, such as 30 mg/d of oral prednisone(Drug information on prednisone), until a clinical remission occurs or for a maximum of 12 weeks.10 In our program, we prefer a "crash course" that starts with 50 to 60 mg/d and decreases thereafter by 5 mg every 2 days to completion.
• Gabapentin(Drug information on gabapentin) (starting as low as 100 mg tid in sensitive or low-weight patients and titrated to a maximum of 3600 mg/d in 3 to 4 divided doses).11 Pregabalin(Drug information on pregabalin) and tricyclic antidepressants (TCAs) used in other models of neuropathic pain can also be of value in CRPS.12 We suggest that pregabalin be started at low doses of 25 to 50 mg/d (particularly in sensitive or low-weight patients) and titrated up to 300 mg bid within a 10- to 14-day period.
For TCAs, the safest strategy is to start at 10 to 25 mg at bedtime ("start low and go slow" in sensitive or low-weight patients) and titrate upward every 5 days to a maximum dose (for analgesia) of 75 to 100 mg.12 Some prefer to go as high as 150 mg at bedtime, but by that time one reaches antidepressant doses. There currently is no evidence to support the use of one TCA over another, but patients may prefer TCAs with lesser anticholinergic effects, such as desipramine and nortriptyline(Drug information on nortriptyline).
• Bisphosphonates such as intravenous pamidronate(Drug information on pamidronate) (a single dose of 60 mg) and oral alendronate (40 mg/d for 8 weeks) have been shown to be effective in CRPS, particularly in the early phases.10
• Topical lidocaine(Drug information on lidocaine) may be useful in the early phases of CRPS.13
• Opioid analgesics can be used to facilitate mobilization of the extremity during physical therapy. Their long-term use may be necessary in refractory cases. However, the clinician must use them wisely given their addiction potential and both short- and long-term adverse effects. The best evidence for opioid efficacy in CRPS is an add-on study of morphine(Drug information on morphine) in patients already treated with spinal cord stimulators.14
• Intranasal (200 to 400 IU/d for 8 weeks) or intramuscular (100 to 300 IU/d for 4 weeks) calcitonin has been shown to have a slight benefit in ameliorating CRPS.10 However, the collective results of 6 randomized controlled trials reported in the literature show that this benefit is comparable with the pain relief obtained by other therapies (eg, physical therapy combined with analgesics).10
• In extreme cases in which patients did not respond to all known interventions, very few have been treated with "ketamine coma."10 The treatment is very aggressive, necessitates intensive care, and remains totally experimental. However, benefit from ketamine(Drug information on ketamine) in CRPS and other intractable neuropathic pain syndromes has been reported in a number of cases.15
Conclusion
In particular, CRPS type 1 symptoms and signs are the result of derangement of the peripheral nervous system and CNS (what in our view constitutes true CRPS) associated with musculoskeletal, endocrinological, and vascular compromise. However, similar presentations can be seen in profound immobilization because of fear of pain and movement; disease imitators (eg, inflammation, tumor, and vascular events), and self-inflicted disorders.20 In the latter case, failing to recognize the self-induced nature of the presentation risks major iatrogenic complications as part of unnecessary and even harmful treatments. Given the complexity and variability of symptoms and signs, every effort should be made to appropriately diagnose the condition as such by using both symptoms and observed signs, as well as inclusion and exclusion criteria.
The prognosis of CRPS 1 and 2 can be variable, depending on a multiplicity of factors, such as magnitude and duration of symptoms/signs, degree of limb guarding or immobility, the presence of CNS changes (in the form of central sensitization or, to the contrary, the presence of expanding sensory hypoesthesia), the degree/intensity of therapeutic interventions, and patient coping factors and psychological/ psychosocial status.
Although science has not yet succeeded in providing full understanding or in reversing the mechanisms that underlie CRPS, most cases are treated successfully by a combination of functional restoration techniques in conjunction with medical and behavioral management.2 Even patients who experience substantial residual symptoms often can regain satisfactory function and good quality of life.




