Diagnosis of isolated axillary neuropathy in athletes: Case studies
Isolated axillary neuropathy is a somewhat uncommon diagnosis, but it may not be as rare as might be expected. Given a thorough clinical history, physical examination, and timely studies, the diagnosis needs to be considered in the differential in the proper setting. Sports and other activities in which this injury might occur include overhead sports (eg, volleyball, javelin), racquet sports, gymnastics, rock climbing, workouts that involve shoulder traction (eg, pullups), and contact sports that involve tackling with an extended arm (eg, rugby, American football).
Isolated axillary neuropathy is a somewhat uncommon diagnosis, but it may not be as rare as might be expected. Given a thorough clinical history, physical examination, and timely studies, the diagnosis needs to be considered in the differential in the proper setting. Sports and other activities in which this injury might occur include overhead sports (eg, volleyball, javelin), racquet sports, gymnastics, rock climbing, workouts that involve shoulder traction (eg, pullups), and contact sports that involve tackling with an extended arm (eg, rugby, American football).
A comprehensive understanding of the anatomy and function is critical to making a definitive diagnosis and formulating an appropriate treatment plan. Most patients with axillary nerve injuries do well with conservative treatment and make a full recovery over a reasonable period; surgical intervention rarely is necessary. In this article, we report cases of axillary nerve injury in an elite teenage baseball pitcher and in a middle-aged recreational cyclist.
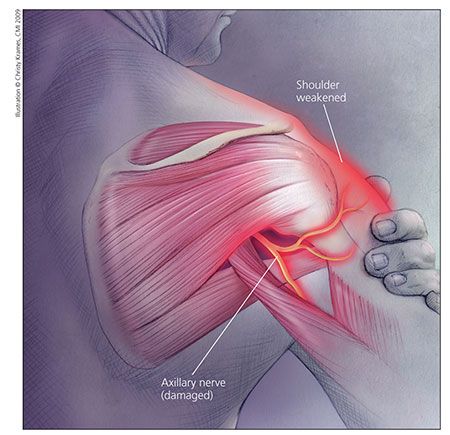
Figure 1 – For axillary nerve injury, a comprehensive understanding of the anatomy and function is critical to making a definitive diagnosis and formulating an appropriate treatment plan. The axillary nerve has its origin at the posterior cord of the brachial plexus and innervates the deltoid and the teres minor. It passes obliquely across the anteroinferolateral aspect of the subscapularis muscle before it enters into the quadrilateral space, accompanied by the posterior humeral circumflex artery. Most injuries arise from closed trauma that involves a traction-type mechanism.
ANATOMY AND FUNCTION
The axillary nerve has its origin at the posterior cord of the brachial plexus (C5-6 nerve roots) and innervates the deltoid and the teres minor. Along its anatomical course, it passes obliquely across the anteroinferolateral aspect of the subscapularis muscle before it enters into the quadrilateral space (QS), accompanied by the posterior humeral circumflex artery (Figure 1).
The QS is defined superiorly by the teres minor (when the vantage point of the shoulder is posterior), anteriorly by the subscapularis, inferiorly by the teres major and latissimus dorsi, medially by the long head of the triceps, and laterally by the proximal humerus.1-3 Within the QS, the nerve lies in close proximity to the inferior shoulder joint capsule and exits posteriorly around the humeral neck. It then splits into the anterior branch (innervates the anterior and middle deltoid bundles) and posterior branch (innervates the posterior deltoid bundle and teres minor). A terminal branch (superior lateral cutaneous nerve) of the posterior branch provides sensory innervation to the lateral deltoid region.2
In axillary nerve injuries, the clinical history is important in determining the cause (Table) and developing an appropriate and timely treatment plan. Most injuries arise from closed trauma that involves a traction-type mechanism. The location of the pain typically is lateral or deep to the shoulder, with occasional radiation to the proximal arm. The pain, which may be mild to severe, often worsens in extreme ranges of motion. The pain tends to be type II neurological pain-dull and aching-rather than the type I “zinger” neurological pain. However, patients often complain of only mild pain and more of weakness or inability to perform in their sport.
On physical evaluation, clinicians need to pay particular attention to the cervical, shoulder, and neurological examinations. Baseline plain radiographs of the neck and shoulder as well as more comprehensive testing (eg, MRI) may be valuable. Nerve testing with electromyography and nerve conduction studies (EMG/NCS) may help confirm the diagnosis and may be needed to monitor the treatment and, ultimately, the recovery process.
CASE REPORTS
Case 1: Elite baseball pitcher
An 18-year-old left-handed elite high school pitcher presented with 3 years of intermittent left arm discomfort. One year before this visit, he had been seen at another orthopedic facility. At that time, a diagnosis of a stress fracture of the left distal humerus was made; the pitcher was treated with casting and rehabilitation.
The patient improved, but his arm was never perfect. He pitched the entire spring and summer seasons but continued to have pain when he threw a lot of hard pitches. The actual number of innings and games he pitched had diminished because of his arm pain. He denied any mechanical or neurological symptoms in the shoulder or elbow. He was otherwise doing fine and was healthy.
Shortly before his initial visit to our office, the patient received an evaluation from a physical therapy group that specializes in elite and professional throwing athletes. A formal analysis of the patient’s throwing mechanics was performed, and corrections were made. He was actively working on making these corrections and noted some improvement in his condition.
On his initial visit to our office, the patient stood 6 ft 0 in tall and weighed 170 lb. He denied any trauma, falls, or surgery. The results of his neurological evaluation were unremarkable, and no atrophy was noted. The shoulder examination demonstrated significantly decreased external rotation, particularly at 90° of abduction. All other specific test results for the neck, shoulder, elbow, and wrist were normal. There was no evidence of tenderness to palpation over the entire upper extremity.
The patient’s primary care physician had ordered an MRI scan of his left arm about a week before the initial visit; the finding was unremarkable. The previously noted stress fracture had healed, and no new findings were noted.
The patient was advised to completely rest the arm, including cessation of throwing, for a few weeks and focus his efforts on his new rehabilitation program. However, he was noncompliant and, against medical advice, he continued to pitch for some college and professional “showcases.” He continued to have pain and, eventually, followed up 4 months after his initial visit with us.
The patient admitted to noncompliance with the medical advice and rehabilitation program. He actually stopped pitching about 4 weeks before this follow-up visit. His examination results essentially were unchanged, and he received the same recommendations.
The patient returned to the clinic 5 months later, having done quite well. His rehabilitation program included aggressive stretching exercises for the shoulder. Twice a day a therapy assistant conducted maneuvers that took the shoulder and arm to the extreme ranges of motion.
The patient’s arm pain had resolved, and he was back to playing baseball and throwing balls from the outfield without difficulty. However, the therapist had not allowed him to return to pitching because during the month before this visit he had noted significant weakness around the left shoulder, especially in the deltoid and external rotator muscle groups. The patient also noticed visible atrophy of the left shoulder. He had no neck pain or radicular-type symptoms. He was healthy and denied any recent illness.

Figure 2 – An elite high school pitcher with axillary nerve injury had significant atrophy of the left deltoid and mild atrophy in the area of the teres minor.
On examination, the patient’s neck was supple, with full range of motion and no pain or stiffness. His reflexes were symmetrical, but he did have slightly decreased sensation over the lateral aspect of his left deltoid. He had significant atrophy of the left deltoid and mild atrophy in the area of the teres minor (Figure 2).
The patient had 4/5 strength on deltoid and external rotator testing of the shoulder. His supraspinatus strength was 5−/5. His external rotation had improved but still was mildly limited compared with that in the right shoulder. All results of stress tests of the shoulder and elbow were negative. The patient had negative Spurling, Hoffman, Tinel, and Phalen test results.
MRI scans of the patient’s cervical spine and left shoulder were ordered, in addition to EMG/NCS of the left upper extremity. The differential at that time included cervical radiculopathy related to a herniated disk; an axillary nerve lesion, perhaps caused by a compressing cyst; and Parsonage-Turner syndrome (PTS).
The MRI scan of the shoulder showed deltoid atrophy but no tears in the deltoid or rotator cuff. The cervical MRI scan revealed only mild disk bulging at C3-4, and the findings were otherwise unremarkable. There was no evidence of spinal stenosis or cervical root compression. The cervical cord was normal, without compression.
The patient’s EMG/NCS test revealed a severe left axillary nerve lesion with significant denervation of the anterior, middle, and posterior deltoid. There was more denervation in the middle deltoid than in the other heads. The middle deltoid had no contracting units. The other 2 heads showed some firing, with the posterior head better than the anterior. This result showed promise for resolution over the following 12 to 18 months. The supraspinatus and infraspinatus muscles were not tested. There was no evidence of cervical radiculopathy or brachial plexopathy.
A neurology consultation was ordered. Similar findings were found on physical examination, with weakness on deltoid and external rotator testing, as well as atrophy as noted above.
The patient was thought to be experiencing an isolated axillary neuropathy probably related to the aggressive stretching program he had undergone during his rehabilitation with the therapist. On the basis of the EMG/NCS findings, his prognosis appeared good, but it was thought that complete recovery might take months.
The patient was advised to avoid intense or prolonged stretching of the left shoulder joint and activities that were associated with his shoulder discomfort. However, he continued with a traditional rehabilitation program for his shoulder. He was instructed to follow up after 3 months for a repeated EMG/NCS test.
The patient did not return for 6 months because he was away at college, but he had done well. His deltoid and external rotator strength had improved dramatically, and his atrophy was nearly resolved. He had no symptoms related to the left upper extremity. He was playing baseball again but decided not to pitch anymore and was focusing his efforts on playing in the outfield for his college team. No further testing was performed, and that was the last time the patient was seen in the clinic.
Case 2:
Recreational cyclist
A 59-year-old right-hand-dominant recreational cyclist presented with a right shoulder injury that he had sustained while riding his bicycle 1 week earlier. A girl riding a bicycle had cut out in front of him; in his effort to avoid hitting her, he locked up the brakes. His momentum caused his body to be thrust forward abruptly, but he did not fall off his bicycle. In the process, however, his right shoulder was jolted and he described feeling a “popping sensation.”
The patient immediately experienced pain and proceeded to have difficulty in lifting his right upper extremity. He had no other complaints, including neck pain, and denied any history of neck, shoulder, or upper extremity injuries or surgeries. This evaluation was his initial one for the injury. The patient had a history of hypertension and hypercholesterolemia, but he was otherwise healthy.
On the initial visit, the patient stood 5 ft 9 in tall and weighed 205 lb. His neurological examination results were unremarkable except for 4/5 weakness in right shoulder abductors and 4−/5 weakness in right shoulder external rotators. He had difficulty with right shoulder active range of motion, especially abduction and forward flexion, but passively his range was full. He had pain on impingement testing, but all other shoulder test results were fine. No atrophy was noted. Results of the patient’s neck and the rest of his upper extremity examination were normal. Findings of plain radiographs of the right shoulder were unremarkable, without fractures or dislocations.
Given the nature of the patient’s injury and clinical presentation, an MRI scan of the shoulder was ordered. Ibuprofen therapy was started, and the patient was instructed to rest the shoulder until follow-up after the MRI scan. The scan revealed only mild rotator cuff tendinosis and no tears. It was otherwise a somewhat normal study.
Because the patient was still experiencing pain, he received a subacromial injection and was instructed to return within 1 week for reevaluation. The injection helped improve his symptoms, but on examination he still had weakness in the shoulder. Because there was concern about a possible brachial plexus injury versus cervical radiculopathy, even though the patient did not have neck pain, an MRI scan of the cervical spine and an EMG/NCS test were ordered.
The MRI scan revealed only minimal degenerative disk disease and no significant stenosis, cord compression, or abnormal signal in the cervical spinal cord. The EMG/NCS test showed evidence of axillary neuropathy but not of right brachial plexopathy or cervical radiculopathy.
A diagnosis was made of isolated axillary neuropathy, probably traction in nature, and a physical therapy program was started for the patient’s shoulder girdle. He was monitored closely over the following several months. Visible atrophy of the posterior shoulder developed in the area of the teres minor but not the deltoid.
The patient made slow, steady progress over the following 6 to 8 months and eventually achieved full recovery of his strength and resolution of the atrophy. He returned to all activities, including cycling, without sequelae.
DISCUSSION
There are few causes of isolated axillary neuropathy; most axillary nerve injuries occur along with injury to the brachial plexus. The typical mechanism of injury is closed trauma that involves traction, often associated with dislocation or fracture. Blunt trauma to the anterior lateral shoulder also may cause axillary nerve injury.2
In our opinion, the athlete in case 1 had a traction injury resulting from overly aggressive stretching during physical therapy.4 The athlete in case 2 also probably had a traction-type injury, this one resulting from the abrupt thrust of his body when he locked up his brakes on his bicycle.
The differential diagnosis included cervical radiculopathy, axillary neuropathy, PTS, brachial plexopathy, and quadrilateral space syndrome (QSS). Although cervical radiculopathy and brachial plexopathy were considerations, no evidence of these diagnoses was seen on EMG/NCS or cervical MRI. Neither athlete had the neck pain usually seen with cervical radiculopathy or the generalized symptoms often associated with brachial neuritis.
The athletes did not exhibit the pattern of PTS that typically includes severe shoulder pain for days to weeks, followed by loss of motor function in the affected muscles. Multiple nerves tend to be involved with PTS, including the axillary, long thoracic, and suprascapular nerves. Of note, the MRI scan did not show increased signal or fatty atrophy in any of the shoulder muscles.
QSS was an important consideration. This syndrome usually occurs with compression of the axillary nerve and posterior circumflex humeral artery within this space by abnormal fibrous bands or muscular hypertrophy of the borders of the space.5 Compression also may occur with lesions, such as glenoid labral cysts.6
In QSS, the EMG/NCS test result usually is normal, and deltoid atrophy and lateral sensory changes are uncommon.2 This syndrome often is characterized by vague, chronic shoulder discomfort and weakness in forward elevation and abduction, with fatigue in overhead positions. Night pain is common.1
On MRI scans, neither athlete had the distinctive and selective teres minor fat atrophy seen in QSS.7 If the athletes had QSS resulting from muscle hypertrophy, we would have expected their symptoms to have improved once atrophy developed in the deltoid or teres minor or both.
We treated these athletes for isolated traction-type injuries of the axillary nerve. The treatment plan included physical therapy, anti-inflammatory medications, and activity modification.8 We advised the pitcher and cyclist to refrain from their respective sports activities while they recovered. In both cases, the symptoms and clinical findings improved and eventually resolved over several months, a typical time frame for recovery.
Surgical intervention may be needed for patients with axillary nerve injuries who do not show improvement after 3 to 6 months of conservative treatment. Repeated EMG/NCS testing also may be necessary.2
References:
References1. Aval SM, Durand P Jr, Shankwiler JA. Neurovascular injuries to the athlete’s shoulder: part II. J Am Acad Orthop Surg. 2007;15:281-289.
2. Steinman SP, Moran EA. Axillary nerve injury: diagnosis and treatment. J Am Acad Orthop Surg. 2001;9:328-335.
3. Burkhead WZ, Scheinberg RR, Box G. Surgical anatomy of the axillary nerve. J Shoulder Elbow Surg. 1992;1:31-36.
4. Haupt HA. Upper extremity injuries associated with strength training. Clin Sports Med. 2001;20:481-490.
5. Cahill BR, Palmer RE. Quadrilateral space syndrome. J Hand Surg Am. 1983;8:65-69.
6. Robinson P, White LM, Lax M, et al. Quadrilateral space syndrome caused by glenoid labral cyst. AJR. 2000;175:1103-1105.
7. Hoskins WT, Pollard HP, McDonald AJ. Quadrilateral space syndrome: a case study and review of the literature. Br J Sports Med. 2005;39:e9.
8. Perlmutter GS, Apruzzese W. Axillary nerve injuries in contact sports: recommendations for treatment and rehabilitation. Sports Med. 1998;26:351-361.





