Article
Diffuse Macular Hyperpigmented Rash and Weakness in an African American Woman
A 46-year-old African American woman was admitted with a 3-month history of extensive macular, nonpruritic, erythematous rash on her upper chest wall.

A 46-year-old African American woman was admitted with a 3-month history of extensive macular, nonpruritic, erythematous rash on her upper chest wall. She also had bilateral proximal upper and lower extremity weakness. Her past medical history was significant for obesity, hypertension, and dyslipidemia.
Musculoskeletal examination revealed decreased muscle motor strength in both the upper and lower extremities but no sensory or cranial nerve deficits. The initial laboratory evaluations revealed leukocytosis (leukocyte count of 12.5 × 103/µL; normal, 3.4 to 9.2 × 103/µL); thrombocytosis (platelet count, 407 × 103/µL; normal, 142 to 405 × 103/µL); and elevated aspartate aminotransferase (71 U/L; normal, 15 to 37 U/L), alanine aminotransferase (81 U/L; normal, 12 to 78 U/L), creatine kinase (921 U/L; normal, 126 to 192 U/L), and aldolase (16 U/L; normal, 1.2 to 7.6 U/L) levels.
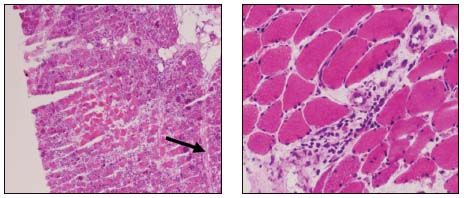
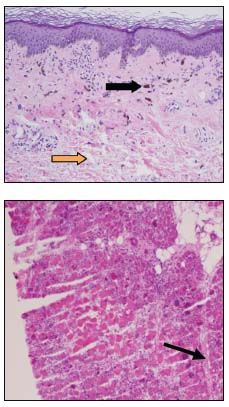
The patient's rash (top, left photograph) and her skin biopsy specimen (top, right photograph) and skeletal muscle biopsy specimen (bottom photographs) are shown.
What is your diagnosis?
(Find the answer on the next page.)
The most prominent feature in the rash photograph is the shawl sign, a diffuse, flat, erythematous lesion that occurs over the upper chest and back and characteristically is seen in dermatomyositis (DM). The skin biopsy specimen (top photograph) showed mucin deposition in the upper dermis (yellow arrow), mild inflammation, and pigment incontinence (black arrow), findings compatible with DM.1 The skeletal muscle biopsy specimen showed a central area of infarcted muscle fibers with surrounding basophilic regenerating muscle fibers (bottom photograph), as well as perifascicular atrophy (black arrow), and sparse chronic perivascular inflammation within the perimysium. The combination of clinical features and pathological changes are consistent with a diagnosis of DM.
Polymyositis (PM) and DM are the most common idiopathic inflammatory myopathies (IIMs). The prevalence of these 2 disorders is about 1 per 100,000 in the general population; there is a female to male predominance of about 2:1. Although persons of any age may be affected, the peak incidence in adults is seen between the ages of 40 and 50 years.
Both PM and DM are characterized by symmetrical proximal muscle weakness and elevated muscle enzyme levels.2 Although cutaneous involvement is specific to DM, each disorder has a characteristic histological finding.
This case highlights the importance of skin and muscle biopsy in confirming the suspected diagnosis of an IIM. Typical findings are perivascular and endomysial inflammation, with accompanying muscle fiber necrosis and muscle fiber regeneration. Endomysial infiltration by chronic inflammatory cells is seen in PM; in contrast, chronic inflammatory cell infiltration develops in perivascular and perifascicular regions in DM. Also, perifascicular atrophy is diagnostic of DM.3 The rheumatologic significance of this case is that although a diagnosis of DM may be suspected with the presence of the typical signs and symptoms, identifying the characteristic pathological findings seen on skin and skeletal muscle biopsy is prudent.
Treatment of patients with PM and DM is tailored toward improving muscle strength and preventing development of extramuscular complications. The initial therapy primarily involves the use of corticosteroids, although a corticosteroid-sparing agent also may be used concomitantly in severely ill patients.
The current first-line corticosteroid-sparing agent usually is azathioprine or methotrexate. It has been suggested that patients who have profound weakness or significant extramuscular complications warrant treatment with 2 drugs from the outset.
The cutaneous manifestations of DM usually respond to the agents used to manage the associated myositis. Although hydroxychloroquine has been shown to be effective in controlling the skin disease in 75% of patients, no benefit for the muscle disease has been seen. Patients should avoid sunlight, use sunscreen, and wear sun-protective clothing because the DM rash often is related to photosensitivity. Topical corticosteroids also may be used for the DM rash.
Therapy with corticosteroids was started for our patient, and improvement was noted within a few days. The patient’s muscle strength increased with physical therapy over the course of the following few weeks. Therapy with methotrexate was started at the follow-up clinic visit, and steady progress in the patient’s muscle strength and skin manifestations was observed.
Problems with/comments about this article? Please send feedback.
References:
REFERENCES
1. Santmyire-Rosenberger B, Dugan EM. Skin involvement in dermatomyositis. Curr Opin Rheumatol. 2003;15:714-722.
2. Dimitri D. Inflammatory myopathies: diagnosis and classifications [in French.] Presse Med. 2009;38:1141-1163.
3. Dalakas MC. Muscle biopsy findings in inflammatory myopathies. Rheum Dis Clin North Am. 2002;28:779-798, vi.




