Article
Doximity Data Show Job Boom in Boston, Growth in Geriatrics
Author(s):
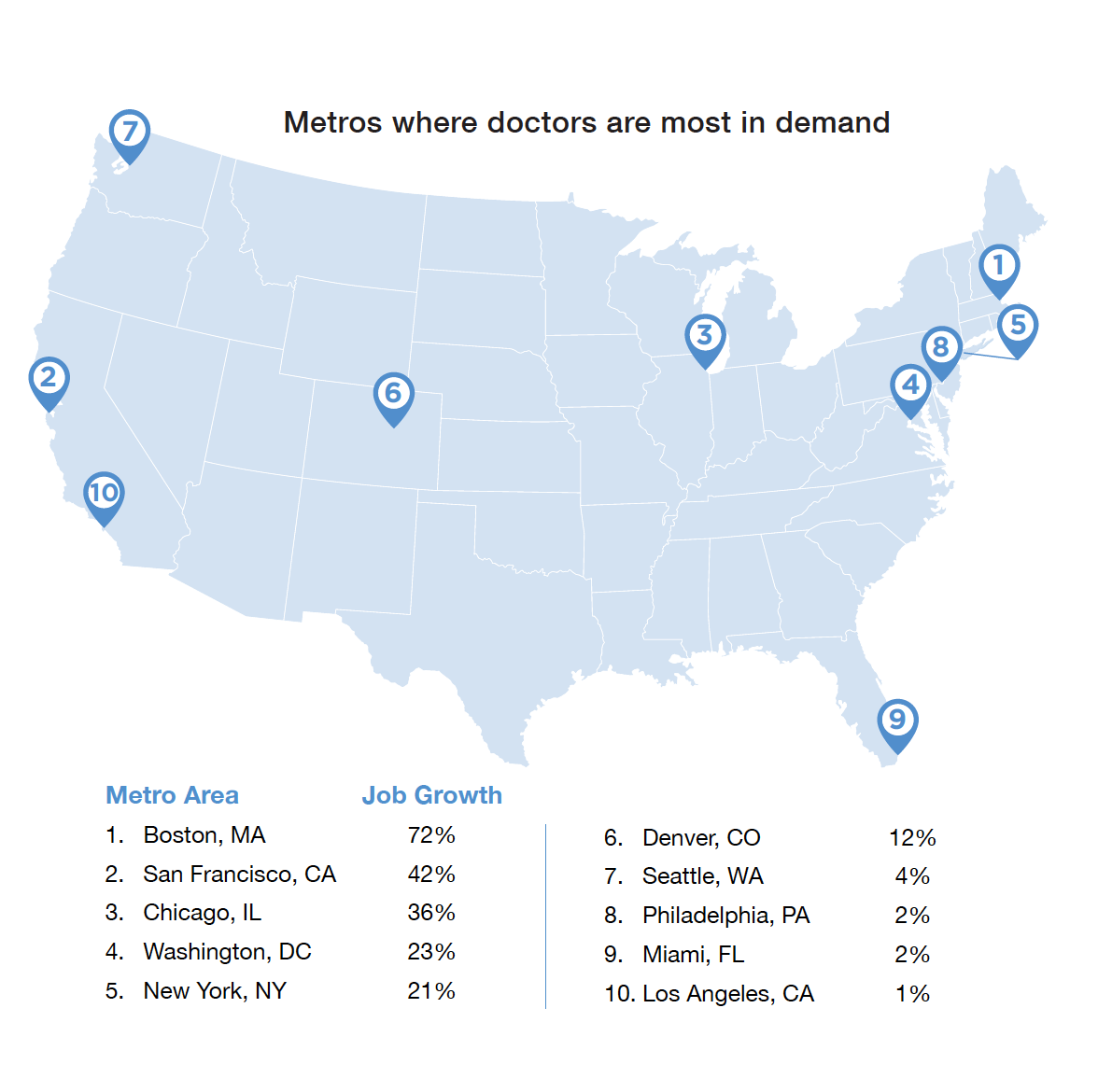
Doximity's US Physician Employment Report 2017 showed the implications of the physician job market in metropolitan areas across the US.

Nate Gross, MD
A report on workforce trends in the medical community from Doximity, the United States’ largest medical social network, has revealed data regarding physician demand, compensation, and implications for specialization in metropolitan areas of the US—most notably Boston, Massachusetts, which saw a 72% increase in job growth, and the field of geriatrics, which saw an increase in jobs of 164%.
The examination was based on more than 12,000 physician jobs posted on the site in 2016 and 2017, including 20 major metropolitan areas and 15 medical specialties. Doximity plays the role of a social networking site, complete with a jobs listing program, for roughly 70% of physicians in the US.
Los Angeles, despite an observed increase in compensation of 13%, was last of the top 10 metropolitan areas in terms of physician demand. The area’s job growth was only 1%, a sharp contrast to its sister city of San Francisco just 300 miles away, which was second in job growth, at 42%.
“I think that really highlights the importance of having granular data,” Chris Whaley, MD, the lead author of the study and an adjunct professor at the University of California Berkley School of Public Health, told MD Magazine. “If we had just looked at the state of California, for example, and tried to look at job growth for the entire state, we’d have missed a lot of that underlying difference for the physician labor market between L.A. and San Francisco.”
While Boston and San Francisco showed the largest increases in job growth, Chicago, Illinois (36%); Washington, DC (23%); and New York, New York (21%) all saw increases over 20%.
Courtesy of Doximity
A physician shortage is expected in the US, with an expected need for 40,000 to 104,000 more physicians by 2030, according to recent research from the Association of American Medical Colleges. The Doximity data showed that physician jobs are expected to grow by 15% from 2016 to 2026.
Part of the reason for the upcoming shortage is due to medical students being more likely to specialize. Another reason is due to the anticipated increase in the average American’s lifespan. Data was in line with that, showing that job growth for geriatrics increased 164%, more than three times any other specialty.
“Each of these specialties will have its own fingerprint based on patient needs on where those doctors happen to be highest in demand,” Nate Gross, MD, the co-founder of Doximity, told MD Magazine. “But as a whole, the number of citizens in this country that are reaching the age where a geriatrician would be helpful in their care has never been higher. The opportunity there has never been greater.”
“From a health policy standpoint, we have known that we are going to need more geriatrics for a long time,” Whaley said. “But what I really like about doing this analysis and this study is that this is the first time that we’ve actually been able to put a real number on that.”
Gross and Whaley noted that while the report did not examine the causation for these data occurring the way they do, there is further insight to be gained from the numbers the study presented.
Urology (49%), oncology (45%), hematology (39%), and obstetrics and gynecology (31%) rounded out the top 5 in terms of job growth. Cardiology saw the smallest increase in the top 10, but still a large increase at 23%. Most of the 15 specialties analyzed saw at least some increase, according to Gross.
The rise of telemedicine and artificial intelligence in medicine have raised fears for a lower demand for real physicians, but according to the data, there is not much hard evidence supporting a lower demand. The technologies do, however, appear to make doctors more productive, showing a trend toward increased enhancement of the physicians’ role rather than one toward replacement.
“Because doctors are getting hired on a network like ours, we can kind of measure where the shortage is being addressed, you could say, and that doctor shortage is huge,” Gross said. “We have a lot of baby boomers that are going to, theoretically, need more care, and our ways to get them care, of course, requires getting the doctor into the right spot. That’s a marketplace.”

Courtesy of Doximity
“It is something that is going to create increases in demand and increases in new job postings or bumps in salary to help motivate doctors to got to the areas where they are most in need,” he added.
In addition to Los Angeles’s 13% pay increase, Indianapolis, Indiana (14%); Philadelphia, Pennsylvania (11%); and Milwaukee, Wisconsin (10%), all experienced pay growth rates of 10% or more. San Francisco saw the highest pay raises, with increases of up to 16%.
Pay declines were shown in 5 major metropolitan areas: Phoenix, Arizona; Columbus, Ohio; Denver, Colorado; Las Vegas, Nevada; and Houston, Texas. Despite the pay decline of -3%, Denver saw a 12% increase in demand for physicians.
The pay data was collected based on self-reported compensation surveys that included an estimated 40,000 full-time and licensed physicians.
“2017 saw another explosive national debate around the funding of healthcare for Americans. What was less controversial but arguably as important, was the growing pressure on medical labor markets nationally,” Gross said in a statement. “Doctors caring for patients is the heart of our system, and we continue to see a big uptick in demand for physicians across the country. This backs up other studies pointing to the possibility of physician shortages moving forward. In the short-term, we’re seeing an impact on physician compensation in our data.”


