Article
Early Detection and Treatment is the Key to Increasing Survival in Patients with Liver Cancer
Author(s):
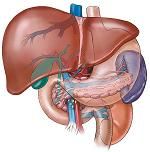
Hepatocellular carcinoma is the fastest rising cause of cancer-related deaths in the United States. However, there are several stages along the way from healthy liver to malignant transformation that offer opportunities for detection and intervention.
Detecting and treating liver cancer at its earlier stages will require a better system of surveillance and testing, said Hashem El-Serag, MD, professor of medicine and chief of the gastroenterology and hepatology section at Baylor College of Medicine during a presentation at a joint conference of the American Gastroenterological Association and the American Society for Gastrointestinal Endoscopy in Coronado, California.
Hepatocellar carcinoma (HCC) is the fastest rising cause of cancer-related deaths in the United States, said El-Serag. The incidence has tripled over the past 20 years.
“Survival really remains dismal” he said, noting that only about 10 percent of people diagnosed with the disease live longer than five years.
Given this stark reality, one way to attack the high mortality rate of liver cancer is to do a better job of implementing a system of surveillance and testing that could lead to early detection, said El-Serag. There are several stages along the way from healthy liver to malignant transformation that offer opportunities for detection and intervention.
“We know most of the risk factors. Hepatitis B accounts for two-thirds of all cases worldwide. Hepatitis C accounts for half of the cases in this country, and alcohol accounts for a very low proportion,” said El-Serag.
In addition, most of the cases seen by doctors have an underlying condition of cirrhosis, an intermediate precursor lesion for hepatocellular carcinoma. Identifying these related medical conditions offer a hypothetical scenario for early cancer detection, said El-Serag.
Guidelines that recommend HCC surveillance are partially based on one of two randomized trials conducted in China. One showed benefits from surveillance and the other did not, said El-Serag.The one that did show a benefit was a larger trial that conducted HCC surveillance using the serum marker alfa-fetoprotein (AFP) in combination with an ultrasound and showed improved mortality among people who were carriers of hepatitis B.
Liver cancer was detected in 86 cases of the screened group and in 67 cases in the control group. There were fewer deaths from HCC in the screened group compared to the control group.
In discussing screening tools, El-Serag noted that while many physicians favor the use of CT scans and MRIs for surveillance they have not been studied for that purpose. Ultrasound is the only imaging modality that has been examined for that purpose, he said.
“When you have someone you suspect has HCC, you do those tests, but bringing in someone who has nothing else wrong with them except being in a high-risk group every six months or 12 months and subjecting them to MRI or CT, that may or may not work.”
In general, tests for liver disease are “ok” but “not great, said El-Serag. However, given the deadliness of the disease, even slightly effective testing if “applied massively and regularly” may help curb mortality, he said.





