Article
Endocrine Case Report: Cirrhotic with Epigastric Pain
Author(s):
The latest case report from Brady Pregerson, MD, features a man in his 60s with a history of diabetes and cirrhosis presenting with 2 weeks of right upper quadrant pain with constipation and 2 days of vomiting. Can you determine the correct diagnosis?
History of Present Illness:
A man in his 60’s with a history of diabetes and cirrhosis presents to the hospital with 2 weeks of RUQ pain radiating to the back with constipation and now 2 days of vomiting. He was triaged as having RLQ pain, not RUQ pain. He denies any fever, bleeding, melena or other complaints.
Vital Signs & Physical Exam:
Vital signs are normal except for a pulse of 101. Physical exam is otherwise normal except for epigastric but not RLQ tenderness
Initial Diagnostic Testing:
CBC: normal except for 79% PMNs
Chem 7: normal except for sodium of 128. LFT’s mildly elevated
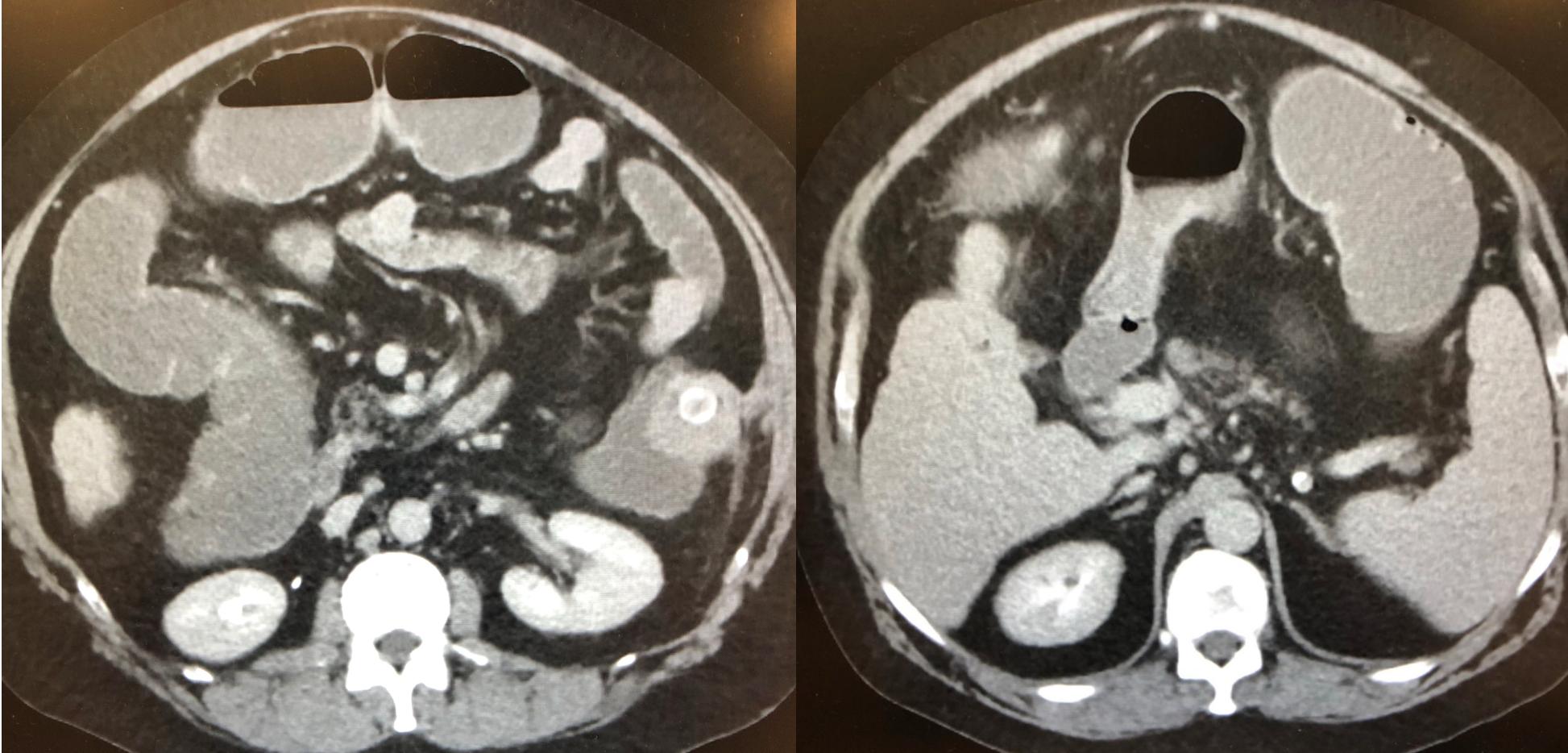
Imaging: A CT scan is done
What is the diagnosis?




