Article
Fecal Microbes Remain 2 Years After Transplant to Treat Clostridium difficile
Author(s):
Certain microbial strains persisted in donor recipients for as long as 2 years after an FMT.
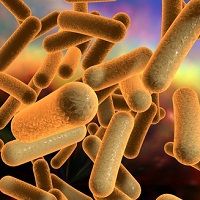
A team of researchers at the University of Alabama at Birmingham (UAB) have shown that microbes from healthy donors can remain in recipients for up to 2 years after a fecal matter transplant (FMT) to treat the diarrhea and colitis caused by recurrent Clostridium difficile infections.
In 2 patients, certain microbial strains persisted for as long as 2 years after an FMT, and another 5 patients showed persistence of the donor strains for 3 to 6 months, the longest times tested, after the transplant.
In combination with a new bioinformatics algorithm, the UAB team of Ranjit Kumar, PhD, Elliot Lefkowitz, PhD, Martin Rodriguez, MD, Casey Morrow, PhD, and other colleagues developed a method to identify related microbes in order to detect the fates of the donor microbes in the recipients. Their method used the detection of single nucleotide variations in microbial genomes.
“It essentially is a personalized microbiome ‘fingerprint,’” Kumar, a research scientist in the UAB Center for Clinical and Translational Science Informatics Institute, said in an article from the university’s press office.
The researchers say that this new method—the first direct demonstration of its kind—may help to explain why, at 90%, FMT has a higher success rate than antibiotic therapy. It may also warn of microbiota changes that may be indicative of metabolic diseases such as obesity and diabetes, digestive diseases such as ulcerative colitis, or even degenerative diseases such as Parkinson’s.
To conduct their research, the team compared variants in short, consecutive windows of DNA sequences that spanned the bacterial genome. In this study, 1,000 base-pair windows were used. The classification model, using the window-based similarity (WSS) data as features, was trained via logistic regression for each bacterial species to identify the statistically significant WSS cutoff value, which was then applied to all possible pairwise comparisons of microbiome sequences from the fecal samples of 6 donors and 7 recipients treated at UAB for C. difficile infection (1 of the donors was used for 2 transplants).
The study samples were obtained 1 to 6 months following transplant, when colonization with donor microbes should have occurred; second samples were available for 2 of the 7 transplants and were collected 2 years following transplant.
Donor microbes were found in recipients’ gut microbiota for all 7 FMTs, measured by the WSS scores above the cutoff for each particular species. In addition, the 2 recipients who were tested at the 2-year mark also showed markers of the donor microbes.
The donor microbes detected in the recipients included 9 species of Bacteroides, 2 species each of Alistipes and Parabacteroides, and 1 species each of Acidaminococcus, Akkermansia, Barnesiella, Coprococcus, Eubacterium, Faecalibacterium, Prevotella, and Ruminococcus.
“In the big picture, people are evaluating certain changes in the human microbiome as a disease predictor,” Lefkowitz, a professor in the UAB Department of Microbiology and director of UAB CCTS Informatics, said. “We have extended the resolution of what we can detect in the gut microbiome, not to just the genus or species, but to individual strain detection.”
Source: University of Alabama Birmingham News
RELATED COVERAGE:
Improving Autism Symptoms with Fecal Matter Transplants
What Types of Patients Will Accept FMT as C. difficile Treatment?
Fecal Transplants Considered as Effective as Antibiotic Treatment for C. difficile Infections