Article
Fecal Transplantation Can Slay Superbugs
Author(s):
Fecal microbiota transplantation (FMT), already shown to be effective for Clostridium difficile treatment, has been found to eradicate two of the most common antibiotic-resistant hospital superbugs: vancomycin-resistant Enterococcus faecium (VRE) and multidrug-resistant Klebsiella pneumoniae.
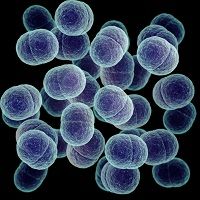
Fecal microbiota transplantation (FMT), already shown to be effective for Clostridium difficile treatment, has been found to eradicate two of the most common antibiotic-resistant hospital superbugs: vancomycin-resistant Enterococcus faecium (VRE) and multidrug-resistant Klebsiella pneumoniae.
A mouse model-focused study published in PLOS Pathogens by Eric Pamer, MD, Memorial Sloan-Kettering Cancer Center, New York, NY, and colleagues investigated whether VRE or K. pneumoniae domination provided resistance against colonization by other pathogens.
Pamer and colleagues simultaneously colonized mice with VRE and K. pneumoniae and treated them with either FMT or a sterile control solution for 3 straight days.
They found that VRE and K. pneumoniae levels were fairly similar within the feces prior to FMT, but had remained elevated in the control group.
However, K. pneumoniae density not only dipped within one day, but also became undetectable within all the mice in seven days.
Additionally, there did not appear to be any competition in intestine domination between VRE and K. pneumoniae. According to the researchers, while the pathogens “peacefully coexisted,” VRE and K. pneumoniae exhibited differences in stimulation and invasion of colonic mucus.
The researchers concluded, “Their findings uncovered previously unrecognized features of VRE and K. pneumoniae colonization and provide insight into the nature of pathogen coexistence, dissemination, and ways to eradicate colonization.”
Moving forward, the team’s research efforts are concentrated on identifying commensal bacterial species — parts of the healthy fecal transplant that allow certain bacteria clearance.




