Article
Fibromyalgia Negatively Impacts Functionality, Quality of Life in Female Patients
Author(s):
Results underline the importance of psychiatric evaluation and treatment in patients with fibromyalgia.
Women with fibromyalgia (FM) were more likely to avoid activity due to pain-induced fear, which intensifies pain and may contribute to its chronicity, according to a study published in Medicine.1 Investigators believe that psychiatric evaluation and subsequent treatment is an important factor in determining functionality and quality of life (QoL) in this patient population.
“In addition to physical complaints such as pain, FM patients have also been shown to experience cognitive dysfunctions such as attention problems, problems in planning, difficulty in remembering, concentration difficulties, decreased vocabulary, poor verbal fluency, mental slowness, difficulty in thinking and making decisions,” investigators explained. “FM syndrome also has many emotional and affective effects. Fibromyalgia syndrome patients tend to experience high levels of stress, anger, and pain catastrophizing and these also contribute to the worsening of existing symptoms.”
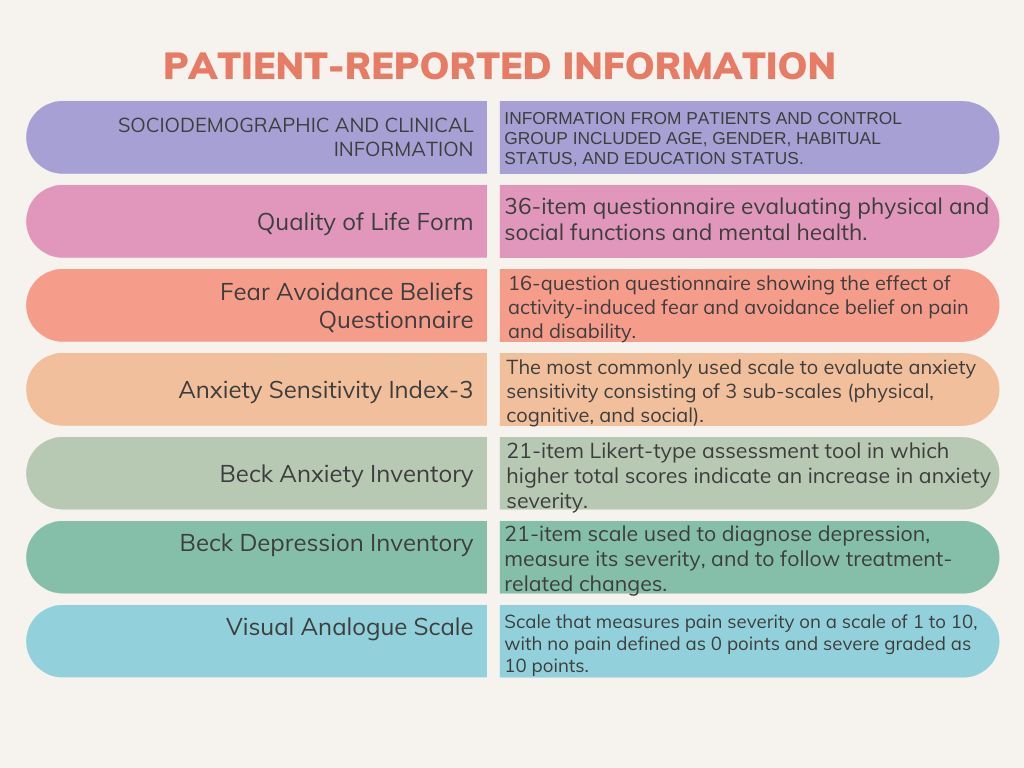
The cross-sectional study analyzed the relationship between FM and depression, anxiety, quality of life, fear-avoidance beliefs, and anxiety sensitivity. In total, 37 female patients with FM who followed up with the Pain Medicine Clinic of the Research Hospital and 37 age- and sex-matched healthy controls were included in the study. QoL and functionality were evaluated via a sociodemographic and clinical characteristics data form, a fear-avoidance beliefs questionnaire (FABQ), Anxiety Sensitivity Index-3 (ASI-3), Beck Anxiety Inventory, Beck Depression Inventory, Quality of Life Form (SF-36), and a Visual Analogue Scale (VAS).
Patients in the FM cohort had statistically lower scores in all QoL subscales, with the exclusion of emotional role difficulty and social functionality scores. Statistically higher scores in physical and work activity subscales in fear-avoidance beliefs questionnaire was also reported. Cognitive symptoms subscale in the ASI-3 (P < .016), the Beck Anxiety Inventory and Beck Depression Inventory, and the VAS scores were also statistically higher (P < .05). Anxiety, depression, and perceived pain severity reduced quality of life and social functionality in this patient population in areas including emotional role difficulties, mental health, and physical function.
The study was limited by excluding male patients. Further, no clinical evaluation was performed regarding psychiatric comorbidities other than the scales and the number of years of FM complaints during the study were not included in the analysis.
“Similar studies determining the effect of AS and fear avoidance behavior on the prognosis of the disease in FM patients are needed in larger samples and different cultures,” investigators concluded. “All these results emphasize the importance of psychiatric evaluation and treatment in FM patients.”
Reference:
Cetingok S, Seker O, Cetingok H. The relationship between fibromyalgia and depression, anxiety, anxiety sensitivity, fear avoidance beliefs, and quality of life in female patients. Medicine (Baltimore). 2022;101(39):e30868. doi:10.1097/MD.0000000000030868




