Article
GERD Patients: Fewer Postoperative Complications Reported with Laparoscopic Anti-Reflux Surgery
Author(s):
GERD patients have fewer postoperative complications with LARS than with OARS.
Patients with gastroesophageal reflux disease (GERD) have experienced fewer postoperative complications when given laparoscopic anti-reflux surgery (LARS) than when undergoing traditional, open anti-reflux surgery (OARS).
LARS patients have also reported faster recovery and lower health care costs.
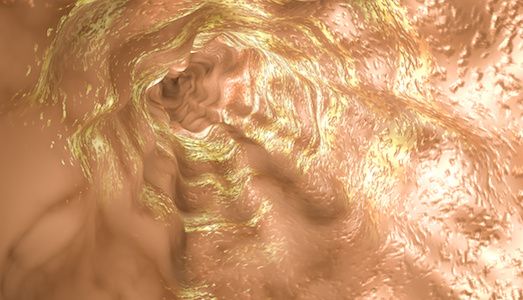
According to Francisco Schlottmann, MD, surgeon at the Center for Esophageal Diseases and Swallowing, University of North Carolina, and the study’s lead author, patients with GERD, a disease that affects approximately 20% of adults in the US, have an “incompetent” lower esophageal sphincter that leads to gastric acid rising back into esophagus.
To better understand the national use of LARS in the US and compare outcomes from post-operation between laparoscopic and open anti-reflux procedures, researchers analyzed information in the National Inpatient Sample (NIS) database, which included 75,544 patients. A total of 44,089 were scheduled LARS and 31,455 had OARS.
According to the study results, patients who underwent laparoscopic surgery were less likely to experience the following reactions: bleeding, cardiac failure, esophageal perforation, death, postoperative blood clots, surgical site infection, and wound complications.
Also, researchers explained that the minimally invasive approach reduced repeated exposure to stomach acid — which could damage the lining of the esophagus and potentially lead to the precancerous condition Barrett’s esophagus.
The minimally invasive approach also appeared to reduce length of hospital stay by approximately two days.
“Anti-reflux surgery should be considered in patients who do not achieve complete control of their symptoms [regurgitation or cough] with medications; who do not want to take medications for the rest of their lives; or who experience complications of medical therapy,” said Schlottmann in a news release.
Marco G. Patti, MD, FACS, surgeon and Director of the Center for Esophageal Disease and Swallowing, University of North Carolina, Chapel Hill, and the study’s senior author concluded in a news release, “Our study highlights the fact that laparoscopic anti-reflux surgery is as effective as the open approach, and in 2017, with all its advantages, should be the standard care.”
The article, “Comparative Analysis of Perioperative Outcomes and Costs Between Laparoscopic and Open Antireflux Surgery,” was published in the Journal of the American College of Surgeons.





