Article
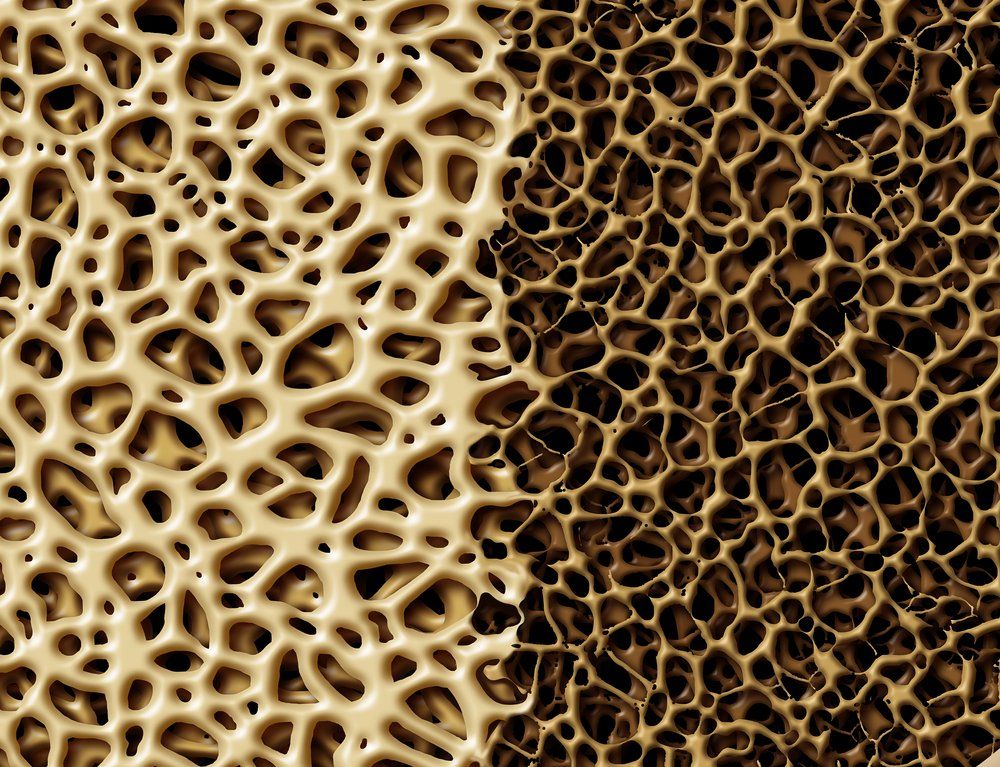
Glucocorticoid Use Results in BMD Loss for Women with Rheumatic Disease
Author(s):
Anti-osteoporotic treatment resulted in increased BMD to a greater extent in patients treated with less than 5 mg per day of prednisone.
The use of glucocorticoid treatment results in a number of improvements for women with inflammatory rheumatic musculoskeletal disease (iRMD).
A team, led by Giovanni Adami, Rheumatology Unit, University of Verona, tested different doses of glucocorticoid treatment in a large cohort of women patients in data presented during the 2022 American College of Rheumatology (ACR) Convergence Meeting in Philadelphia.
In the longitudinal cohort study, the investigators examined 884 women with inflammatory rheumatic musculoskeletal disease, including rheumatoid arthritis, systemic lupus erythematosus, psoriatic arthritis, systemic sclerosis, and other rheumatic diseases.
The majority of participants were diagnosed with rheumatoid arthritis. The study also included 1766 control participants matched for age, T-score, and the percentage 10-year fracture risk. Each patient was followed up with for up to 6 years.
The glucocorticoid intake for each patient was between 0-2.5 mg per day pred eq mean dose, 2.5-5 mg pred eq mean dose or ≥5 mg per day pred eq mean dose.
The team assessed bone mineral density and fracture prospectively and compared them to a 2:1 propensity score matched cohort of healthy women.
They also developed Kaplan-Meier curves with log-rank tests for iRMD’s stratified for glucocorticoid use and dosage and matched cohort respectively. Finally, they employed multivariable Cox regression survival models to analyze the effect of glucocorticoids on fracture.
The results show BMD levels decreased significantly in all patients treated with glucocorticoids that were not receiving anti-osteoporosis treatment (-4.26%, P = 0.0011; -4.23%, P = 0.0422; -2.66%, P = 0.0006 for ≥5 mg/day, 2.5-5 mg, and 0-2.5 mg/day, respectively).
However, anti-osteoporotic treatment resulted in increased BMD to a greater extent in patients treated with less than 5 mg per day of prednisone.
There were 21, 12, and 29 fractures reported for patients receiving ≥5 mg/day, 2.5 mg to 5 mg and 0 to 2.5 mg/day respectively. This corresponds with a crude fracture rate of 4.8 fractures per 100 person-years, 2.8 fractures per 100 person-years, and 2.5 fractures per 100 person-years respectively.
Ultimately, 103 fractures were registered in the PSM cohort with a crude fracture rate of 2.2 fractures per 100 person-years. The fracture incidence was also higher in patients with iRMD compared to the control group.
Glucocorticoid use of at least 5 mg per day was linked to a 2-fold higher risk of fracture of any kind compared to all other doses and controls (aHR, 2.37; 95% CI, 1.33-4.23).
“GC doses as low as 2.5 mg/day were associated with BMD loss in iRMD but this effect was preventable with anti-osteoporotic drugs,” the authors wrote. “The latter finding might support anti-osteoporotic treatment initiation in patients taking very low-dose GCs, in direct contrast with most guidelines of GIOP.”
The study, “Impact of Glucocorticoid Dosing and Anti-Osteoporotic Treatment on Bone Health in Patients with Inflammatory Rheumatic Musculoskeletal Diseases: A Longitudinal Cohort Study,” was published online by ACR Convergence.




