Article
On GUARD: A Web Tool That May Predict 3-year Diabetes Risk
Author(s):
Inpatient hyperglycemia found on admission blood tests can be explained by medications, stress reaction, or, “Other.” When is “other” a red flag for diabetes? A new online tool from Scotland may help answer that.
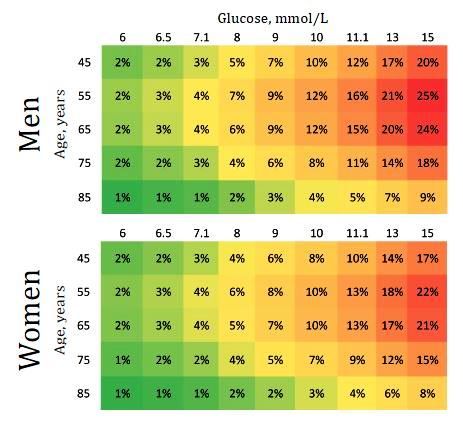
Illustration only of GUARD risk prediction grid based on McAllister et al, 2014.
Hyperglycemia on hospital admission is linked to worse outcomes, including increased mortality.1 Medications, such as corticosteroids, thiazides, phenothiazines,and beta-agonists can be to blame and so can glucose elevation related to stress hormones. Inpatient hyperglycemia can also be a harbinger of future diabetes.2
Just how predictive is it?
A team of researchers in Scotland addressed that question in a study recently published in PLoS One Medicine.3
The retrospective cohort study looked at incident T2DM after emergency hospital admission with hyperglycemia in Scotland between 2004 and 2008. Data came from a Scottish national database of hospital admissions linked to a national register of diabetes.Patients with prevalent diabetes (diagnosed within 30 days of discharge) were excluded.
The 3-year risk of developing T2DM was stratified by admission glucose, age, and sex. Key results for participants age 40 years and older are summarized in the Table.
Table.
aWorld Health Organization
NB: An independent validation cohort of over 22,000 people showed “good discrimination” with a C-statistic of 0.75 (95% CI 0.73-0.76)
The authors found that the 3-year risk of T2DM was <1% for patients with a glucose of ≤5 mmol/L and increased linearly to approximately 15% at 15 mmol/L; above this no further increase was seen. The 3-year risks at the World Health Organization diabetes diagnostic cut-points for fasting (7 mmol/L) and random (11.1 mmol/L) glucose were 3% and 10%, respectively.
Predictive tool
The researchers used this information to develop an online risk predictor tool called GUARD (Glucose on Unselected Admissions and Risk of Diabetes) that uses age, sex, and hospital admission glucose to estimate a patient’s 3-year risk for T2DM.
The authors point out in introductory comments that there are tools to help primary care clinicians determine whether risk of T2DM is high enough to warrant a blood glucose test. Factors used in these calculators include demographic, lifestyle, and anthropometric characteristics. But there is no corresponding calculator that will interpret risk associated with an abnormally high glucose level detected on a routine blood panel ordered after hospital admission. Is it related to medication? Stress? Other? This renders physicians unable either to advise patients on the clinical significance of raised glucose during acute illness, or to decide what if any follow-up testing is appropriate
“Our tool provides an additional way of identifying those patients at high-risk for type 2 diabetes, allowing clinicians to offer lifestyle advice and testing as appropriate” commented first author David McAllister, Clinical Lecturer in Epidemiology and Public Health at the University of Edinburgh. The accuracy of the online tool is “similar” to questionnaire-based methods of predicting diabetes risk, according to McAlister.
The online calculator, McAllister explained, can be used to estimate risk in countries where the risk of T2DM is similar to that in Scotland (2% in persons older than age 40 years). In countries with different background risks, he adds, most patients with high admission glucose will not develop T2DM since the underlying cause is more likely to be stress hyperglycemia or other transient problems. The risk of T2DM in these patients, however, is “not trivial,” and they may still require follow-up, he pointed out.
“The tool may be particularly useful in patients who are unable or unwilling to attend preventive services, but who have contact with medical services as a result of hospitalization,” McAllister emphasized.
A note on study limitations: Race/ethnicity and BMI data not were included; researchers could not determine whether glucose was measured in a fasting or nonfasting state; results have not been tested in nonwhite populations outside Scotland.
References:
- Umpierrez GE, Isaacs SD, Bazargan N, et al. Hyperglycemia: an independent marker of in-hospital mortality in patients with undiagnosed diabetes. J Clin Endcrinol Metab.2002;87:978-982.
- Dungan KM, Braithwaite SS, Presier JC. Stress hyperglycemia. Lancet. 2009;373:1798-1807.
- McAllister DA, Hughes KA, Lone N, et al. Stress hyperglycemia in hospitalized patients and their 3-year risk of diabetes: A Scottish retrospective cohort study. PLoS Med. 2014;11: 1-18.




