Article
Hip Pain in a Patient With Lupus
A 29-year-old African American woman came to our rheumatology clinic with right hip pain that had been getting worse for the past 3 months. She had been diagnosed with systemic lupus erythematosus (SLE) 2 years earlier. She reported excruciating right hip pain and mild pain in her left hip on weight bearing and, occasionally, at rest.
The Case:

A 29-year-old African American woman came to our rheumatology clinic with right hip pain. She had been given a diagnosis of systemic lupus erythematosus (SLE) 2 years earlier. She reported excruciating right hip pain and mild pain in her left hip on weight bearing and, occasionally, at rest. The hip pain and limitation of mobility had been worsening over the previous 3 months, she said.
Since her diagnosis with SLE, she had been receiving oral prednisone, 60 mg/d, and oral mycophenolate mofetil, 750 mg twice daily, for the SLE. The pain in her right hip began 1 year after starting these medications.Clinical Findings:Medical History:
• SLE
• Hepatic abscess
• Cholecystectomy
• Hypertension, resulting from SLE
• No reported history of cigarette smoking or IV drugs; occasional alcohol consumption
Medications:
• Oral prednisone, 60 mg/d, and oral mycophenolate mofetil, 750 mg twice daily, for SLE
• Aspirin
• Ibuprofen
• Metoprolol
• Furosemide
• Amlodipine
• Losartan
• Multivitamins
The patient denied the use of any other over-the-counter supplements.
Physical Examination:
• Blood pressure: 130/86 mm Hg
• Heart rate: 88 beats/min
• Temperature: 37.1°C (98.8°F)
• Respiratory rate: 18 breaths/min
Cushingoid appearance (facial puffiness) and truncal obesity
Musculoskeletal Examination:
• Pain elicited by passive internal and external rotation of the right hip
• No external deformity or tender points were noted
• No butterfly rash, diskoid skin lesions, joint effusions, or synovitis
Laboratory Test Results:
• C3 complement: 91 units (normal, 86 to 184)
• C4 complement: 20.2 units (normal, 20 to 59)
• Thyroid-stimulating hormone: normal
• Antinuclear antibody titer: 1:160 (normal, < 1:40)
• Smith antibody: 405 units (normal, 0 to 49)
• Complete blood cell count: normal
• Creatinine: 2.99 mg/dL (normal, 0.7 to 1.7)
• Erythrocyte sedimentation rate: 14 mm/h
• Antiphospholipid antibody titer: normal
For an x-ray image of the hip, see the next page.Radiology:
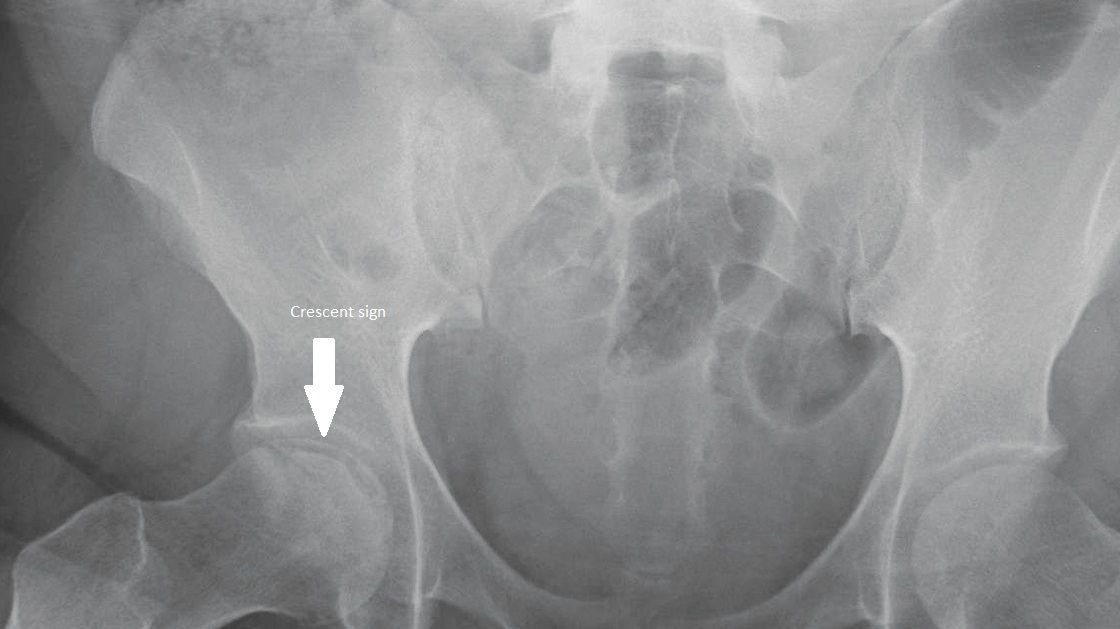
Anteroposterior (AP) view of the patient’s pelvis. Note the crescent sign.What is your diagnosis?
(Find the answer on the next page.)
Diagnosis:
Osteonecrosis of the femoral head.
The diagnosis was based on the patient’s history of high-dose corticosteroid use and physical examination and radiographic findings, and was later confirmed with MRI.
(See Discussion on the next page.)
Discussion:(References are at the end of the final page.)
Our patient’s chief complaint was hip pain. The most common causes of hip pain in adults are fracture of the femoral head, osteonecrosis of the femoral head, strains of various muscles and tendons that are attached to the femoral head, bursitis, osteoarthritis, and inflammatory joint diseases.1
Osteonecrosis, first described in patients with SLE by Dubois and Cozen,2 is thought to result from temporary or permanent loss of blood supply to the bones. Without blood, the bone tissue dies and causes the bone to collapse. This disease is also known as avascular necrosis, aseptic necrosis, and ischemic bone necrosis.
Osteonecrosis is a major cause of morbidity in patients with SLE. Corticosteroid use has been suggested to be the main causative factor. However, osteonecrosis has long been recognized in patients with SLE who did not have previous exposure to corticosteroids. The cause of osteonecrosis in SLE is thought to be multifactorial.
Our patient had been receiving high-dose corticosteroids for 1 year before we saw her. Cushingoid habitus secondary to the treatment also had developed.
Patients who receive high doses of corticosteroids and become cushingoid have been shown to be more likely to have osteonecrosis with SLE.3 Other causes of osteonecrosis of the femoral head are listed on the next page.
Causes of Osteonecrosis
• Systemic corticosteroid use
• Excessive alcohol intake
• Renal transplant
• Systemic lupus erythematosus and other autoimmune diseases
• Chronic liver disease
• Burns
• Pregnancy
• Trauma, including femoral neck fracture and history of previous trauma
• Metabolic diseases (eg, diabetes mellitus, hyperlipidemia, gout, Gaucher disease)
• Sickle cell disease
• Hemoglobinopathies
• Coagulopathies
• Caisson disease
• Pancreatitis
• Radiation
• Chemotherapy
• Congenital diseases (eg, Legg-Calv-Perthes disease, slipped capital femoral epiphysis)
Most patients with osteonecrosis of the femoral head have slowly progressive hip pain that may increase on weight bearing and walking. The pain may progress for weeks and months without any radiologic changes. Pain usually is located in the groin and radiates down to the medial thigh. Pain at rest, a sign of advanced-stage osteonecrosis, is attributed to elevated intraosseous pressure.
In the early stages, range of motion is normal. In advanced stages, joint destruction leads to limitation of extension, internal rotation, and abduction. Clinical signs are atypical. Limping and atrophy of the rectus and gluteus muscles are nonsensitive signs of pain-related disuse of the joint.
Radiologic studies are the most helpful in making the diagnosis of osteonecrosis. Early diagnosis may be made by spotting changes in the femoral head on MRI and radionuclide bone scanning. MRI now is considered the “gold standard” for early diagnosis of osteonecrosis.
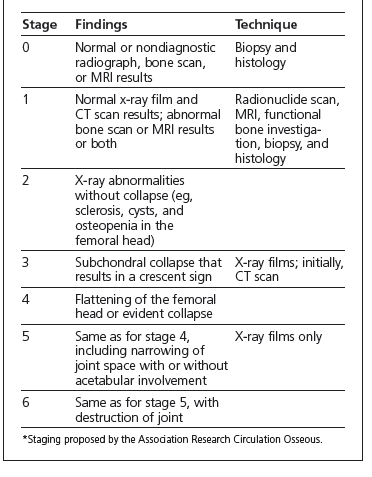
In the later stages of disease, radiography alone generally is sufficient for making the diagnosis. In the AP view (left), our patient showed a crescent sign, or linear lucency along the margin of the femoral head (arrow). The crescent sign is a stage 3 finding in the staging proposed by the Association Research Circulation Osseous for osteonecrosis of the femoral head (below).4,5
Treatment options vary according to the stage of disease. Nonoperative therapy includes administration of NSAIDs, reduction of weight-bearing activities, and elimination of risk factors. However, nonoperative management of osteonecrosis of the hip in adults often leads to poor results.
Core decompression has been reported to have a notable effect on the natural history and clinical progression in the early stages of osteonecrosis. It provides effective management for both non–corticosteroid- and corticosteroid-associated osteonecrosis other than in cases with SLE involvement, in which it is associated with a higher rate of progression to total hip replacement.6
Another form of treatment is flexion osteotomy of the proximal femur. Total hip replacement is the procedure of choice for patients in the later stages of disease (stages 3 to 6).1Outcome:
Our patient’s prednisone was tapered and, eventually, stopped. We discontinued the NSAIDs because of her chronic renal insufficiency.
At the time of this writing, the patient was awaiting an orthopedic evaluation for total hip replacement.
This case was submitted by Advitya Malhotra, MD, and Tina Kochar, MD, residents, and Emilio B. Gonzalez, MD, professor and director of the division of rheumatology, department of medicine, all at the University of Texas Medical Branch in Galveston.
More from the Journal of Musculoskeletal Medicine
References:
1. Zacher J, Gursche A. Regional musculoskeletal conditions: “hip” pain. Best Pract Res Clin Rheumatol. 2003;17:71-85.
2. Dubois EL, Cozen L. Avascular (aseptic) bone necrosis associated with systemic lupus erythematosus. JAMA. 1960;174:966-968.
3. Mok CC, Lau CS, Wong WS. Risk factors for avascular bone necrosis in systemic lupus erythematosus. Br J Rheumatol. 1998;37:895-900.
4. Steinberg ME, Hayken GD, Steinberg DR. A quantitative system for staging avascular necrosis. J Bone Joint Surg. 1995;77B:34-41.
5. ARCO (Association Research Circulation Osseous), Committee on Terminology and Staging: the ARCO perspective for reaching one uniform staging system of osteonecrosis. In: Schoutens A, Arlet J, Gardeniers J, et al, eds. Bone Circulation and Vascularisation in Normal and Pathological Conditions. New York: Plenum Press; 1993:375-380.
6. Maniwa S, Nishikori T, Furukawa S, et al. Evaluation of core decompression for early osteonecrosis of the femoral head. Arch Orthop Trauma Surg. 2000;120:241-244.




