Article
How Providers Can Improve Care For Transgender Patients
Author(s):
As more physicians are caring for transgender patients, many are finding they are unprepared and they lack the training, skills, and resources to do so, according to the authors of a recent review article.

Nicole Rosendale, MD
As more physicians are caring for transgender patients, many are finding they are unprepared and they lack the training, skills, and resources to do so, according to the authors of a recent review article.
There are changes to improve acute care for transgender patients that can be made at the provider level, along with systems-based changes like a more inclusive health care system and more inclusive research, said lead author Nicole Rosendale, MD, Department of Neurology, Priscilla Chan and Mark Zuckerberg San Francisco General Hospital and Trauma Center, and University of California, San Francisco.
“It's important for providers to understand that they will care for transgender individuals, if they have not done so already, and that historically this is a community that has not received the equitable care it deserves,” said Rosendale. “As providers, we should strive to provide high-quality, evidence-based health care to all of our patients.”
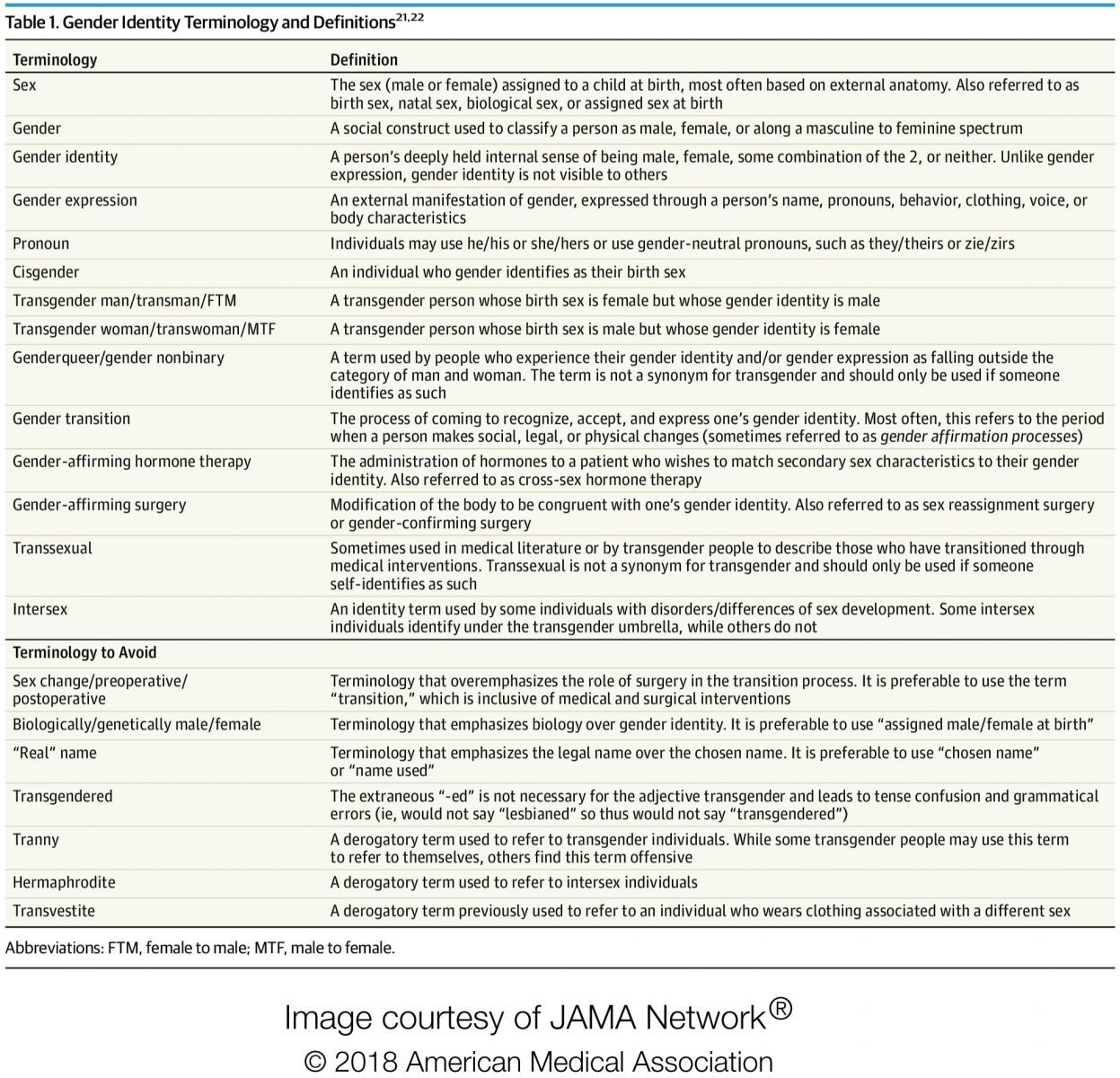
Rosendale and her colleagues emphasized the correct use of language in their review, and included a list of basic terminology with which providers should be familiar. These include terms like “gender,” “gender identity,” and “gender expression,” along with definitions of how those terms differ. Perhaps just as valuable is the list of terminology to avoid, which is also included.
Looking at the clinical considerations, the authors recommend taking an “anatomic inventory” to understand if the patient has undergone any gender-affirming surgical procedures such as facial feminization, breast or chest surgery, vaginoplasty, or other surgeries (all of which are listed in a figure in the article). Rosendale and colleagues stressed that this information can be valuable as the patient may be dealing with possible complications related to these surgeries.
Another clinical consideration is the possibility that the patient is taking gender-affirming hormone therapy, including estrogens, antiandrogens, and testosterone. Gender-affirming care such as hormone therapy is considered medically necessary by many institutions, including the American Medical Association; however, their use may elevate the patient's risk of certain conditions, including hypertriglyceridemia, osteopenia, venous thromboembolism (VTE), or other conditions.
“During a hospitalization, outpatient hormone therapy should be continued, even if it is not on the hospital formulary,” wrote the authors. “Alteration or discontinuation of gender-affirming hormone therapy should involve a discussion of potential risks and benefits with the patient or surrogate, informed by the current limited data from transgender populations.”
Although this review article may be helpful as an introduction to best practices in caring for transgender patients, Rosendale encouraged providers to find additional training.
“The most immediate step providers can take is to seek out training in trans-inclusive communication and care,” said Rosendale. “The majority of providers did not receive formal training in transgender medicine in school, and it is important to get that training so they are aware of how best to care for their transgender patients.”
Rosendale pointed to training options for providers offered by The Fenway Institute and the Gay and Lesbian Medical Association.
In addition to training for individual providers, the authors state that there are steps needed to make the entire health care system more inclusive for transgender patients. They point to the need for a dedicated space in electronic health record systems to note a patient's preferred name and pronoun.
Additionally, the authors pointed to the need for more data about the transgender population.
“It is also going to be difficult to truly understand the needs of the transgender community when gender identity is not obtained in national surveys,” explained Rosendale.
Information about the potential risks of hormone therapy and data to inform accurate interpretations of laboratory values for transgender patients are especially important.
“Within the acute care setting, one of the more immediate needs is to rigorously study what effect, if any, gender affirming hormones have on [the] risk of venous thromboembolism, both peri-operatively as well as within the inpatient setting in general,” said Rosendale.
The review includes a table of laboratory values physicians should be aware of including creatinine, LDL cholesterol, and triglyceride levels; however, changes that could be observed in results for transgender women and men who are receiving hormone therapy are listed in general terms such as “increased,” and “increased or no change or decreased” along with the studies that provide those guidelines. The need for more research in this area is clear.
Despite the significant hurdles that remain in advocating for better care for transgender patients, Rosendale said the most important take away is that individual providers can make changes to better serve the transgender patients in their care.
“Although there is a dearth of high-quality data in transgender care and there are a number of barriers within the health care system for transgender individuals, there are steps providers can take towards achieving the goal of an equitable level of care for their transgender patients,” said Rosendale.
The study, “Acute Clinical Care for Transgender Patients,” was published in JAMA Internal Medicine.




