Article
Hypertriglyceridemia Increases Recurrent Stroke Risk, Despite Statin Use and Well-Controlled LDL-C
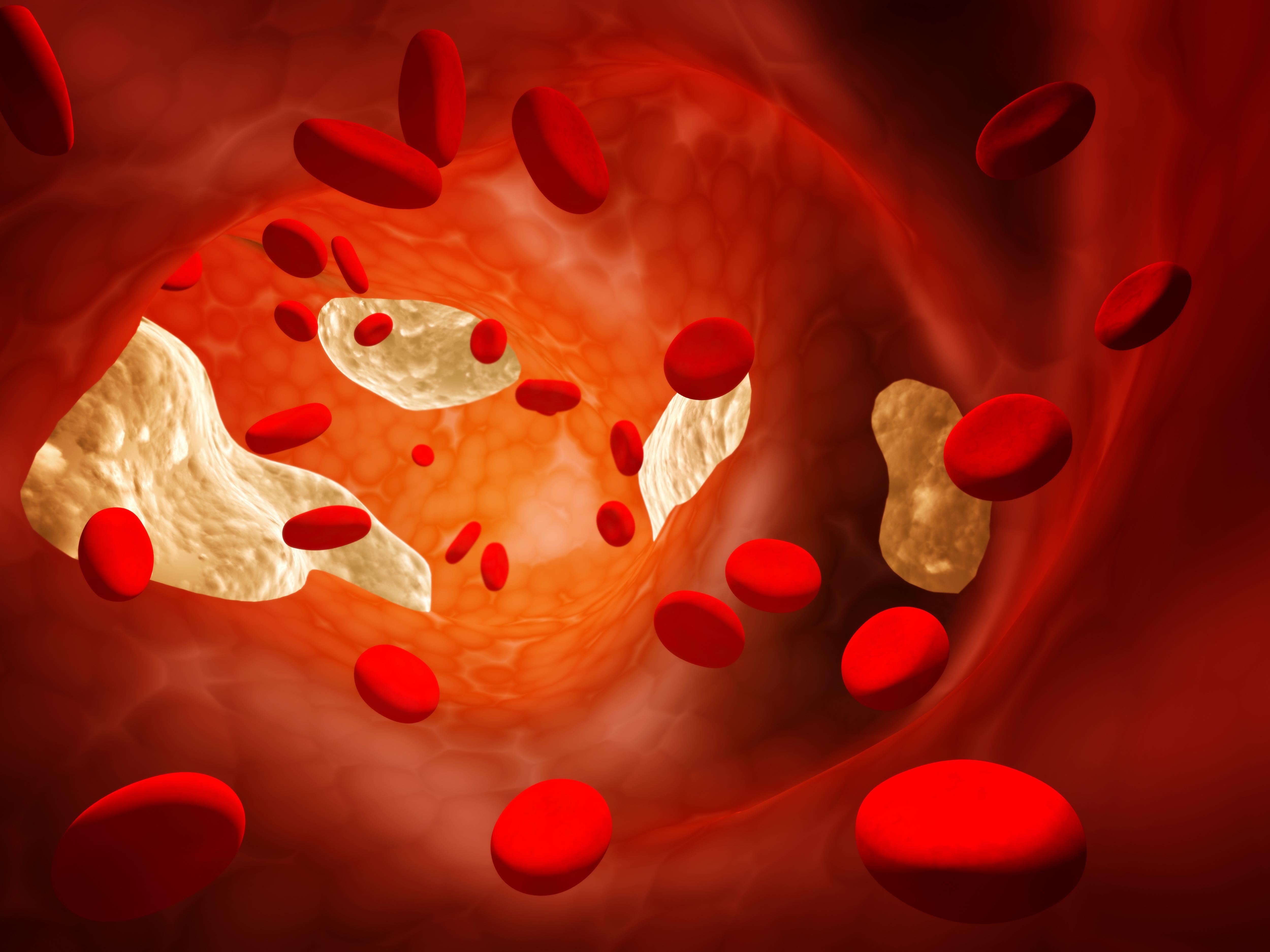
Presence of hypertriglyceridemia was associated with a more than doubling in risk of recurrent stroke among patients with a history of stroke, even after adjustment for LDL-C levels and statin use.
An analysis of data from 870 patients with acute ischemic stroke or TIA from an ongoing prospective, observational registry, results of the study provide insight into the prognostic value of hypertriglyceridemia, particularly among patients with a history of stroke of atherothrombotic origin.
“Our study suggests that for people who had atherothrombotic stroke, having elevated levels of triglycerides in their blood is a risk factor for having another stroke or other cardiovascular problems in the future, and we found that to be true even if the person is on statin therapy,” said study author Takao Hoshino, MD, of the Tokyo Women's Medical University in Japan, in a statement. “The good news is that statin medications are just one therapy for high triglycerides—diet and exercise can also be effective ways to reduce the levels in your blood at little or no cost.”
As the focus on the role of triglycerides in lipid management continues to evolve, hypertriglyceridemia has become a focal point for interest among lipidologists and prevention specialists. Citing a lack of knowledge surrounding associations between hypertriglyceridemia and atherothrombotic stroke, investigators designed their study to assess how hypertriglyceridemia might contribute to residual risk among patients with a history of stroke of atherothrombotic origin.
To do so, the investigators’ study leveraged data from the Tokyo Women’s Medical University Stroke Registry, which is an ongoing, prospective, observational, single-center registry consecutively enrolling patients with acute ischemic stroke or TIA. From the registry, investigators identified a cohort of 882 patients who underwent eligibility assessments from December 2014-January 2020. Of these, 8 were excluded because their final diagnosis was a stroke mimic or more than a week had elapsed since stroke onset and 2 more were excluded for not having lipid profile data at baseline.
The final study cohort included 870 patients, with 784 experiencing stroke and 86 experiencing TIA. The mean age of this cohort was 70.1years, 60.9% were male, and 24.9% had hypertriglyceridemia, which was defined as serum triglyceride levels of 150 mg/dL or greater under fasting conditions. Compared to their counterparts without hypertriglyceridemia, those with hypertriglyceridemia were younger, more likely to be men, have obesity, have diabetes, and to consume cigarettes and alcohol. Investigators pointed out there were no significant differences in usage rates of statin or vibrates among those with and without hypertriglyceridemia.
The primary outcome of interest for the study was a composite of major adverse cardiovascular events, which included nonfatal stroke, nonfatal acute coronary syndrome, and vascular death. Investigators also noted plans for subgroup analyses, including among patients with stroke of atherothrombotic origin.
Of the 870 patients included in the final analyses, 105 experienced at least 1 vascular event within the first year, which correlates to an event rate of 12.5% (95% CI, 10.4-14.9%). Results of the analysis indicated patients with hypertriglyceridemia were at a significantly greater risk of major adverse cardiovascular events (HR, 2.46 [95% CI, 1.62-3.74] P <.001) and any stroke (HR, 2.24 [95% CI, 1.41-3.54]; P=.001) than those without hypertriglyceridemia. In analyses of those with stroke or TIA of atherothrombotic origin, those with hypertriglyceridemia were at a significantly greater risk of major adverse cardiovascular events (HR, 3.59 [95% CI, 1.76-7.33]; P=.001) and any stroke (HR, 3.29 [95% CI, 1.50-7.22]; P=.003) compared to those without hypertriglyceridemia.
“More research is needed, but for people who have had an atherothrombotic stroke, triglyceride levels may emerge as a key target for preventing future strokes and other cardiovascular problems,” Hoshino added. “Statin therapy is still an effective treatment for people with high triglyceride levels, but our study highlights how important it is to look at all the tools a person can use to lower their triglycerides, including diet modifications, exercise and taking omega-3 fatty acids.”
This study, “Prognostic Role of Hypertriglyceridemia in Patients With Stroke of Atherothrombotic Origin,” was published in Neurology.




